Long before COVID-19, there was the Babylon flu epidemic in 1200 B.C.E. Then came the Plague of Athens in 429 B.C.E, the Justinian Plague in 541 C.E., and the Bubonic Plague in the mid-14th century, which scored the highest death toll in human history. Then, in the 1910s, the ill-named Spanish flu pandemic hammered the global population. In the last century, we’ve also seen the scourges of polio, HIV, measles, SARS, and Ebola.
Outbreaks wax and eventually wane, and they typically follow a similar pattern. The COVID-19 pandemic will likely be similar, although after two deadly years, it’s been difficult to chart a path forward. But public health leaders are still trying, in spite of the virus’s rapid evolution. On a panel at the World Economic Forum last month, Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases and the president’s chief medical adviser, broke down COVID’s endgame into five phases: pandemic, deceleration, control, elimination, and eradication. “I coined [them] based on historical experience with outbreaks, together with my own personal experience,” Fauci later tells PopSci. “History repeats itself. I was trying to put it in perspective on what our historical experience has been with pathogens—particularly viruses—that have threatened society.”
[Related: How to tell when the COVID pandemic is nearing its end]
Labelling the phases of the pandemic is an important way to communicate with the broad public about next steps, says Lauren Sauer, a public health researcher at University of Nebraska Medical Center. Although she cautions against rigidity in the absolute definitions, “using phrases like these can help us initiate a conversation—help us roadmap where we are.”
Drawing from history and the latest COVID research, here’s what Fauci and his peers think the rest of the pandemic might look like.

True pandemic
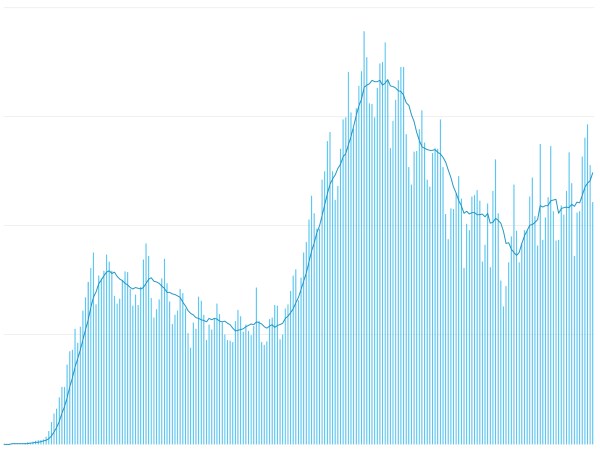
According to Fauci, the first phase of a widespread outbreak is the “pandemic” stage. That’s what the world’s been contending with for the past two years: social instability, uncontrolled community spread, the collapse of healthcare systems, and mass deaths. Since SARS-Cov-2 first crossed US borders in early 2020, the pandemic has infected more than 76 million people in the country (about a fifth of the population) and claimed nearly 900,000 lives.
In these dark times, the country never emerged from the pandemic, with dips in cases followed by variant-triggered surges.
Deceleration
Now that the Omicron wave has broken over many parts of the world, the US and other countries are seeing cases decline. If this downward trend persists, we will arrive at the “deceleration” phase. Improvements in several health metrics, including hospitalization rates, daily case counts, and death rates, should indicate that the worst is over. Fauci says this is where the nation might be right now, though other researchers say it’s still too early to know for sure. In New York City, for instance, the average new COVID cases have dropped to less than a tenth of their peak since the first week of January, and the death count has plateaued. States such as Florida and Alaska are reporting a steady decrease in the average daily cases by population. In South Africa, where Omicron was first detected, the average cases counts are almost 90 percent lower than the peak in December 2021, prompting the government to partially lift COVID restrictions.
As Sauer notes, this phase is hard to identify early on; it’s easier in hindsight to know that we’re in it.
Control
After a sustained deceleration, countries can wade into the control phase of the pandemic, also known as the endemic stage. During this time, people can incrementally drop the strictest precautions and return to normal at large. The virus will still lurk among us, dangerous but manageable. There be local blips in cases, but they won’t spread out of hand.
The work doesn’t end in the control phase, however. People have to stay vigilant to tackle cases whenever and wherever they pop up. It’s like Whac-A-Mole, but instead of a hammer we use vaccines, tests, and post-infection treatments.
Elimination, then eradication
Elimination and eradication occur when a virus is stamped out of a country—and then the entire world for good. With no more outbreaks, the disease becomes a distant memory that future generations need not worry about.
These last two phases, Fauci says, are not realistic goals for COVID. While the US has eliminated polio and measles (although vaccine hesitancy has led to a resurgence in the recent decade), the viruses haven’t been eradicated because they still percolate beyond our borders. There’s only one disease that’s been successfully eradicated in humans: smallpox in 1980.
The virus behind COVID doesn’t lend itself to elimination or eradication, says Monica Gandhi, an infectious disease physician at the University of California, San Francisco. “It’s the hard truth, but it’s something that we have to admit,” she explains. Unlike smallpox, SARS-Cov-2 fails in all the requisite categories (or succeeds, from its own evolutionary perspective). For one, COVID symptoms are too similar to ones from other respiratory illnesses, which prevents us from identifying and isolating patients with necessary speed. What’s more, the pathogen is just too infectious and has a relatively long incubation period, with some strains stretching up to two weeks or 20 days in severely infected patients. This means the virus can be spread before people are even aware that they’re sick.
Also of note, we don’t have a vaccine that provides lifelong immunity against the virus. A COVID infection won’t guarantee safety, either: Omicron, for example, had a mutation that allowed it to re-infect people. And finally, even if we manage to protect each individual of the virus, it can still travel through furry hosts like white-tailed deer and household pets, only to evolve and strike humans again. The ongoing mystery of the virus’s animal origins further complicates our understanding of its footprint across the natural world—along with our attempts to thwart future outbreaks.
Navigating the rest of the pandemic
“The best we can hope for is a very adequate degree of control,” Fauci says, when asked what’s next in the fight against COVID. He likens it to our tenuous truce with the flu, which we’ve learned to function with and work around. As Fauci puts it, the US should shoot for a manageable infection rate with COVID that’s on par with common respiratory diseases such as the flu.
Fauci emphasizes that the country is still nowhere near the control phase, with hospitalizations and deaths at “unacceptable” levels. More than 300,000 new cases are popping up in the US daily, and the death toll is climbing closer to one million. Despite the overall decline in outbreaks, healthcare systems across the nation are strained; some states have had to mobilize the National Guard to help in hospitals, testing centers, and even classrooms. While “acceptable” is a nebulous metric, Fauci stresses that we need to reach an infection rate low enough to take the pressure off vulnerable populations: the elderly, the immunocompromised, and the very young. “I want to make sure that people appreciate that you don’t accept the concept of living with the virus when it is at such a high level,” he says.
That means COVID endemicity is even further off—though experts do have some clue as to how we might get there. The key is a more transmissible, and more importantly, milder variant like Omicron, says Gandhi. Projections show that by March 2022, 60 percent of the world population will be infected with Omicron. “That’s providing a huge wall of immunity,” Gandhi says, though it may not last longer than a year.
Gandhi points out that COVID’s progression has echoed the 1918 influenza pandemic in some ways. Back then, after the crush of the first two waves, a new variant led to a third and final surge; researchers today suspect that it was a more contagious, but milder strain. That, plus the development of flu vaccines in 1942, might have eventually brought us into the control phase that continues today.

But that’s just “the best-case scenario,” Fauci says. “There’s also a worst-case scenario: if we get a new variant that eludes immune protection.” Seeing SARS-CoV-2’s versatility so far, there’s reason to think Omicron could give rise to an even more virulent strain. “With the immune protection that we currently have in society, I would say it’s unlikely,” Fauci says. “But we must be prepared for it.”
Other experts call for a hardline approach in dealing with Omicron, deceleration or not. The US has a zero track record when it comes to predicting the downturn of the pandemic, says Julia Raifman, a public health expert at Boston University. She cites the government’s decision to rescind indoor masking and social distancing policies last May, thinking that the worst was over. But the country has lost 300,000 more people to COVID since July, and there could be another surge around the corner, especially if infection is seasonal, like with other common respiratory diseases. “We’ve had far too much overconfidence,” says Raifman. “We have to have humility about this new virus in our midst and all that it has already destroyed.”
[Related: We already know how to keep the next pandemic from catching us off guard]
Sauer agrees that we shouldn’t think the pandemic peak has come and gone, now matter how promising the fall in current infection rates seems, or how fatigued the world is. “Part of the message is to continue to fight a little longer,” she says. “As we get closer to what feels like an out in the pandemic, we need to continue to push to get everyone across the globe vaccinated, and not give up on people who have not gotten vaccinated yet.”
Vaccination is certainly a means to control, but the current shots might not get us there. COVID researchers say that each booster provides diminishing returns on enhancing immunity, and it’s unlikely that people will keep signing up to get them. And though non-mRNA vaccines could provide a workaround for regular boosters, experts like Fauci agree that the greater goal is to build up immunity right now, so we can outstrip the pace at which the virus evolves.
Ultimately, the distinction between pandemic and endemic is murky; the labeling of phases predicts an end to the pandemic, but not necessarily an end in sight. The US is already significantly more prepared now than it was in March 2020, with the rollout of vaccines for nearly all age groups, large-scale dispatch of free tests and masks, and multiple options for treatments and antiviral pills. What we have to do now is work through global vaccine inequity and reach the control phase together. While humanity might never achieve total peace with the virus, the goal is at least to no longer be at constant, full-blown war with it.