This post has been updated. It was originally published in March 2021.
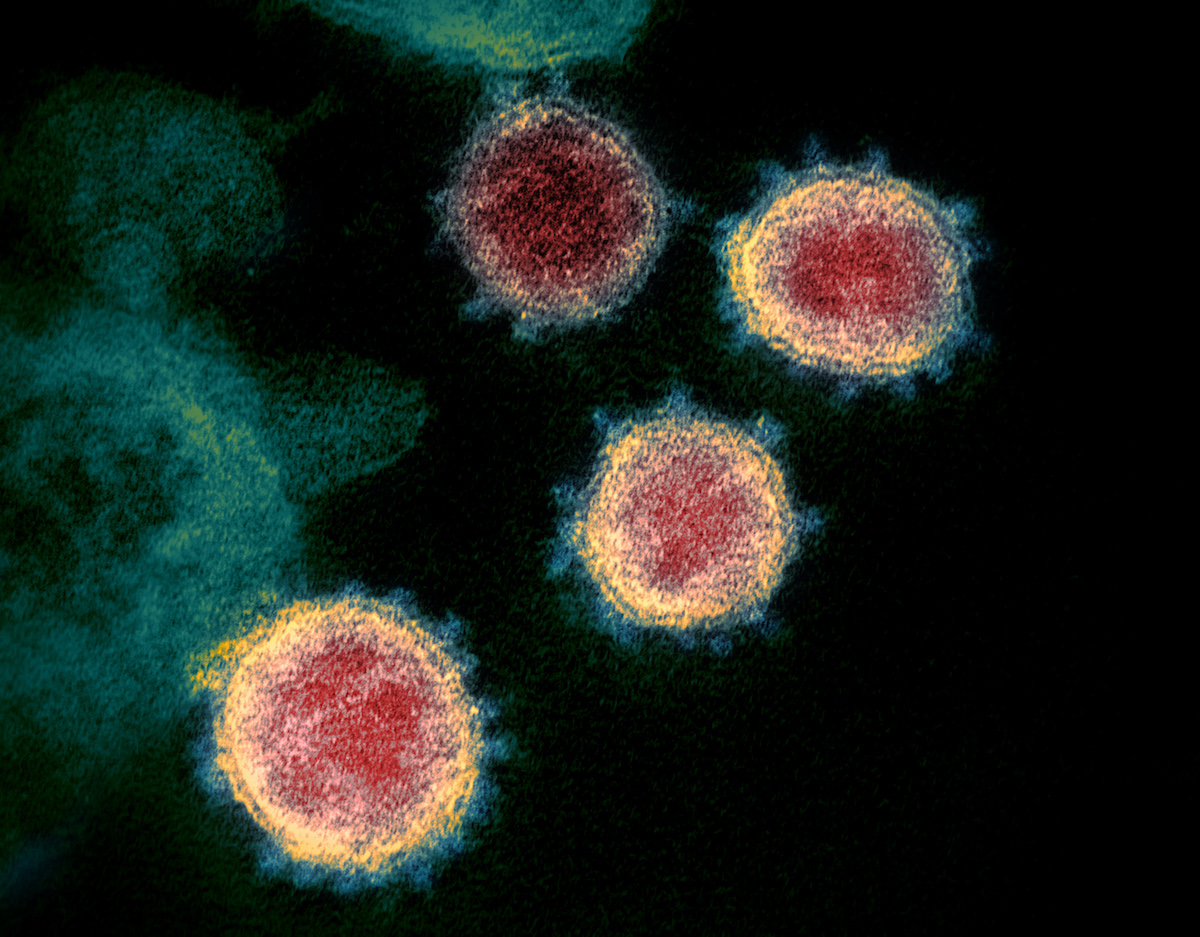
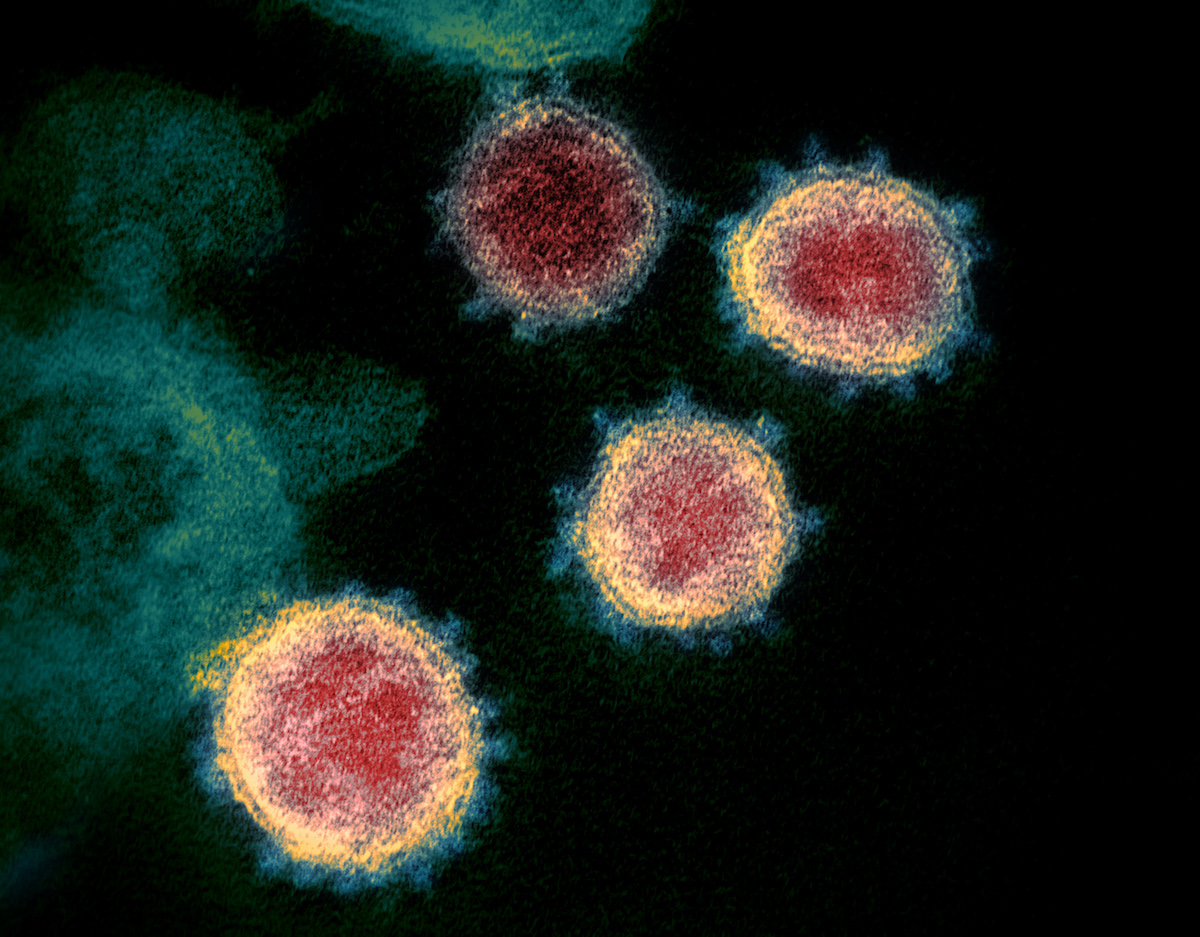
If there’s one thing we can count on in life, it’s change, and viruses are no exception. Variants of the original SARS-CoV-2 virus have popped up in different corners of the world. That might sound scary, but it’s actually perfectly normal, or even “humdrum” as one Nature study puts it.
While virologists predicted all along that the virus that causes COVID-19 would mutate, it’s impossible to predict exactly how deadly or transmissible the next one will be. Some variants, like Delta and Omicron, are more infectious than previous strains. Omicron is currently the dominant form of COVID in the US, largely because it can infect people who have recovered from earlier waves of the disease. Globally, a small but rising proportion of cases are stemming from a sub-lineage of Omicron, BA.2, which preliminary research has found to be more transmissible and possibly more deadly. In the US, however, so many people have been infected by Omicron that BA.2 is unlikely to lead to a new COVID surge.
Here’s what you need to know about COVID mutations.
BA.2: A sub-lineage of Omicron
As Omicron spread in Europe, a particular strain of the variant, called BA.2, began to take off much faster than other versions. In January, it spread widely in Denmark, and drove waves of infection in the Philippines and India. On January 23, the UK officially designated BA.2 a “variant under investigation. The World Health Organization (WHO) states that the sub-lineage is more contagious than prior variants, and one Danish study estimated a 30 percent transmission advantage over other Omicron strains.
In addition to its possible increased transmissibility, BA.2 has lost a key mutation that characterized the original Omicron variant. That feature allowed certain PCR tests to distinguish Omicron from other strains, and means that BA.2 will be slightly harder to identify, hence the nickname “stealth Omicron.”
More concerningly, early research published in mid-February found that in hamsters, BA.2 was more likely than other Omicron lineages to cause weight loss and low blood oxygen—signals that it could make humans dangerously sick. But virologists who study disease severity cautioned against putting too much weight on the findings, both because animals are an imperfect predictor of virus behavior in humans, and because most people who are infected will have immunity from vaccines or prior infection. “You should probably redouble whatever efforts you now take to protect your pet hamster,” one expert wrote on Twitter. “BA.2 Omicron is tough on them. Whether it’s tough on humans, [we] don’t know yet.”
That same study found that BA.2 was less susceptible to the one monoclonal antibody treatment still approved in the US, though not entirely resistant. People with three doses of mRNA vaccines should still be able to neutralize the virus, however.
BA.2 also doesn’t seem to reinfect people who’ve already had another form of Omicron, meaning that it probably won’t trigger a COVID wave in the US. Preliminary findings out of Denmark found that of the 187 Danes who were reinfected by the coronavirus in a two-month span this winter, just 47 cases involved Omicron followed by BA.2, “mostly in young unvaccinated individuals with mild disease.” Even if BA.2 has a transmission advantage, it won’t have room to spread if most people have recently been sick with another lineage. Real world data backs that up: As of February 19, the Centers for Disease Control and Prevention (CDC) attributes under 10 percent of COVID cases in the US to BA.2.
Omicron: The world’s dominant variant (B.1.1.529)
On November 26, 2021, WHO declared a variant first identified in South Africa and Botswana to be “a variant of concern.” By early January, the variant caused more than 90 percent of COVID-19 cases in the United States.
The variant has a large number of variations, including about 30 mutations in the spike protein and 50 mutations throughout the rest of the virus. The spike mutations in particular allow it to dodge the immune system’s first line of defense.
“There is now consistent evidence that Omicron is spreading significantly faster than the Delta variant,” WHO director-general Tedros Adhanom Ghebreyesus said in a briefing in December of 2021. “And it is more likely people vaccinated or recovered from COVID-19 could be infected or re-infected.”
While it’s absolutely normal for viruses to mutate, researchers are concerned because they haven’t seen this combination of changes in the SARS-CoV-2 virus yet. Further, mutations in the spike protein are always cause for concern, as that’s the area of the virus that current vaccines target. Pharmaceutical companies that make the vaccines—Moderna, Pfizer, and Johnson & Johnson, among others—have found that a booster dose confers strong protection against illness, and some are testing variant-specific updates for future boosters.
Omicron cases appear to have a lower risk of hospitalization and death, although record-setting infection rates mean hospitals were crushed by a wave of new admissions at the start of the new year. However, it’s still not clear if the variant is intrinsically milder, or if prior immunity from infection or vaccination is simply keeping it from sickening and killing people. New research from the Imperial College London showed that Omicron is more than five times likelier to cause reinfection, isn’t necessarily milder than the Delta variant, and that two-dose vaccines are not very effective against infection, though they do offer strong protection against serious illness. Vaccine effectiveness against symptomatic illness, according to the study, is 0-20 percent after two doses, and 55-80 percent after a booster dose.
“This study provides further evidence of the very substantial extent to which Omicron can evade prior immunity given by both infection or vaccination,” author Neil Ferguson and Imperial College London medicine professor said in a statement. “This level of immune evasion means that Omicron poses a major, imminent threat to public health.”
While vaccines may not completely halt Omicron’s spread, it’s crucial that Americans who aren’t already vaccinated and boosted get their shots immediately, as this could make the difference between a quick recovery at home and death. To stay safe, continue with tried and true methods to prevent transmission—even if you’re vaccinated—like wearing masks, frequently washing your hands, and social distancing.
Delta: The variant that originated in India (B.1.617)
The Delta variant, a spin-off of the B.1.617 lineage which also includes Kappa, was first identified in India in October 2020, and has since spread around the world. Delta was the most common variant in the US until Omicron came along, and has been shown to be incredibly transmissible—even more so than the common cold. Scientists have estimated that the original strain of the novel coronavirus had a reproductive number (R0) of about 1.5 to 3.5, meaning each sick person infects, on average, another one to four people. The delta variant, though, seems to be even more infectious than that. Researchers estimate that each sick person will infect about seven people. That makes it twice as infectious as the original strain and almost as contagious as the chickenpox.
Experts are still determining whether or not Delta makes people sicker than other variants, but almost all hospitalizations and deaths due to the variant are in unvaccinated populations.
“As older age groups get vaccinated, those who are younger and unvaccinated will be at higher risk of getting COVID-19 with any variant,” Inci Yildirim, a Yale Medicine pediatric infectious diseases specialist and vaccinologist, said in a press release. “But Delta seems to be impacting younger age groups more than previous variants.”
The lineage that includes Delta and Kappa is known for two major mutations—E484Q and L452R, the first of which may help the virus evade antibodies, according to The New York Times.
COVID patients in India, where the variant has been especially prevalent, experienced rarer symptoms like stomach pain, nausea, vomiting, loss of appetite, hearing loss, and joint pain. Ganesh Manudhane, a Mumbai cardiologist, told Bloomberg in June that he has seen increasing cases of microthrombi, which are clots in small blood vessels, so severe that gangrene develops, which can be life-threatening.
“I saw three to four cases the whole of last year, and now it’s one patient a week,” Manudhane told Bloomberg.
There were also concerns about vaccine efficacy against the Delta. One study showed that two Pfizer doses were 88 percent effective against Delta, compared to 93 percent effective against the UK-originated Alpha strain. One study found that the J&J vaccine may be less effective at fighting off Delta, too.
Delta-plus: A sub-lineage of the Delta variant (AY.4.2)
Another variant that’s been of recent concern among virologists is what’s known as the Delta-plus variant. Scientists are describing this version as a sub-lineage of Delta, according to The New York Times, which essentially means it is most closely related to that variant and likely evolved from it. Delta-plus has a spike protein mutation that researchers have also identified in the Beta variant (described below).
The variant likely originated in India but has now spread to other countries, including the United States.
Some experts believe this variant is even more transmissible than the highly transmissible Delta variant, though more research is needed to confirm this. “It is most likely capable of dodging immunities,” Shahid Jameel, a virologist and director of the Trivedi School of Biosciences at Ashoka University in Sonipat, India, told The New York Times in late June. “That is because it carries all symptoms of the original Delta variant and also from its partner Beta variant.”
Alpha: The variant that originated in the UK (B.1.1.7)
The COVID-19 variant first detected in the UK—also known as B.1.1.7—was identified on December 14, 2020, causing tightened lockdown rules and border control inside the UK and between other countries. The virus has been found more frequently in southern England, and what has stood out to researchers most is a large number of mutations it’s taken on—a whopping 23 shifts from the original COVID-19 virus that emerged from Wuhan, China, in late December 2019.
This variant spread to the United States earlier this year, and was doubling around every 10 days back in January 2021, according to one preprint study. Delta accounted for more than 90 percent of US cases by August 2021, however, and Omicron overtook Delta in December 2021.
While scientists believe that the COVID-19 vaccines currently being distributed are still effective against this version of the virus and there’s no change in disease severity compared to the original, the B.1.1.7 version is thought to be more contagious. According to the BBC, this variant has the ability to spread between 50 and 70 percent faster than previous forms of the virus.
Beta: The variant that originated in South Africa (B.1.351)
A few days after the discovery of the Alpha variant, another—known as B.1.351—popped up in South Africa that displayed similar mutations. It quickly became more dominant than earlier variants throughout the country, nearly replacing the other versions in the Eastern Cape, Western Cape, and KwaZulu-Natal provinces.
Similar to Alpha, the Beta variant doesn’t necessarily make people get more sick, but it certainly appears to be more transmissible.
Research over the past several months has been done to test out the efficacy of the vaccine against this variant. Back in January, according to Reuters, scientists at BioNTech, the German biotech company that partnered with Pfizer to develop one of the vaccines currently in use, said they were testing the vaccines against the new variants and, if needed, could make tweaks in as little as six weeks.
Gamma: The variant that originated in Brazil (P.1 lineage)
The Gamma lineage was spotted in four people in Japan after they took a trip to Brazil. It developed late in 2020 in Brazil’s Amazon region, becoming dominant there, and in surrounding South American cities. By January 2021, the variant had also been found in parts of Europe, as well as in Oklahoma and Minnesota.
A close cousin to the Beta variant, Gamma has similar mutations, including what virologists have dubbed the E484K mutation, which affects the spike protein and may make it trickier for certain vaccines to provide maximum effectiveness. Another major worry, reports NPR, is that of reinfection rates. The number of mutations on P.1 variants can theoretically help the virus evade antibody response, which may be why Manaus, Brazil, saw a resurgence of this particular strain.
“If you were to ask me right now, what’s most concerning of all the things that I’ve heard so far, it’s the fact that they are reporting a sudden increase in cases in Manaus, Brazil,” University of Massachusetts virus expert Jeremy Luban told NPR. “Manaus already had 75 percent of people infected [in the spring of last year].”