Can popping a Motrin or Advil stop your heart? Possibly, according to a study published earlier this week in the European Heart Journal Cardiovascular Pharmacotherapy.
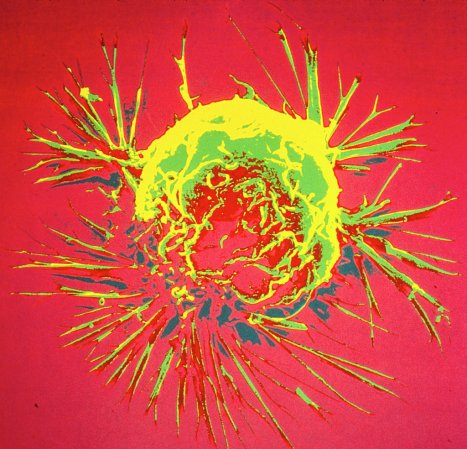
The study found that people who take certain Non-Steroidal Anti-Inflammatory Drugs (better known as NSAIDs) were more than 30 percent more likely to experience cardiac arrest. Although cardiac arrest and heart attacks are often used interchangeably, strictly speaking a cardiac arrest is when your heart stops beating—a heart attack is when oxygen is blocked from entering your heart, which often leads to cardiac arrest.

Diclofenac, a prescription pain reliever often used for arthritis and migraines, and ibuprofen (often sold as Motrin and Ibuprofen in the United States) were the riskiest drugs, while Naproxen sodium (sold as Aleve) and the prescription pain reliever Celecoxib (sold as Celebrex) were the safest.
To assess each pain reliever’s relationship to cardiac arrests, Danish researchers pulled data from 28,947 Danish residents who’d experienced a cardiac arrest outside of a hospital from 2001 to 2010. Denmark, which has had universal healthcare since the 1960s, started the Danish Cardiac Arrest Registry in 2001 in an attempt to reduce the number of cardiac arrests and improve patient outcomes. It contains the anonymized data of every cardiac arrest patient since the database’s inception. The research focused on out-of-hospital cardiac arrests (OHCAs) because people already in hospitals often have illnesses or other confounding factors that could cause their heart to stop.
Researchers used a technique known as the case-time-control method, that allows subjects to effectively function as their own control group.
“In that way we circumvent the problem with all kinds of confounders with diseases,” said lead study author Katharine B. Sondergaard. “Do they smoke? Are they obese? Do they have hypertension? All of these kinds of things we can’t control are eliminated because the patient controls himself.”
To rule out whether any correlative effects were related to say, a new drug being used more often, the study authors put together a control group of 115,788 participants from the Danish Patient Registry that were demographically similar to the case group, then put them through the same analysis. They then used statistical analysis to compare the two groups.
While they found that use of any NSAIDs increased the overall risk of cardiac arrest, not all NSAIDs were equally dangerous. Diclofenac was associated with a 50 percent increase in risk, while ibuprofen was associated with a 31 percent increase. Aspirin, which is an NSAID that’s thought to be heart-friendly because of its blood thinning effect, was not included in the study.
It’s important to note that these drugs only increase a person’s underlying risk. If a patient had a two percent chance of a cardiac arrest before taking diclofenac, the drug would only increase their total risk to three percent. But this isn’t the first study to suggest that there could be a link between NSAIDs and heart ailments, or even stroke.
“And the problem,” said Sondergaard, “is that for a lot of people, a cardiac arrest is their first symptom of heart disease. You could be walking around with a heart disease and you don’t know it until you suddenly have a cardiac arrest.” So you might not realize that you’re at high risk of cardiac arrest when you start popping pills.

It’s scary to think that the drugs we routinely turn to for safe pain relief might actually make us sick. There are strong parallels to the realization a few years ago that acetaminophen (aka Tylenol) can cause spontaneous liver failure at relatively low doses or when mixed with alcohol.
That’s why Sondergaard thinks that people should have a doctor examine them before they start taking NSAID’s. That said, because of their anti-inflammatory effects, NSAIDs in particular are often a go-to drug for women dealing with menstrual cramps. Because menstruating women are generally young and healthy, a couple of ibuprofen for a day or two are unlikely to stop their heart. But they should take less than 1200mg a day, and should avoid taking them for more than a day or two. Earlier studies on heart attacks found that people developed symptoms after as a little as a week on NSAIDs, but the fact remains that risk is lower for younger people.
Still, Sondergaard said, “You don’t have to take it on an everyday basis to be at risk from the drug.”
And even the drugs deemed safe in this particular study aren’t necessarily harmless. For example, people who took reofecoxib didn’t have an uptick in cardiac arrests. But in the United States, reofecoxib—sold as Vioxx—was pulled from the market in 2004. Its manufacturers had found that chronic use could cause heart attack (which differs from cardiac arrest) and even stroke.
The takeaway? Get regular check-ups to keep tabs on your heart health, know your personal risk factors, and don’t mindlessly take medication just because it didn’t require a prescription.
“When you sell these drugs in supermarkets and stuff,” said Sondergaard, “you signal that it’s a safer drug that you can take without risk. And that’s just not the truth.”