Sniffle season is here, but so is a potential solution—and we don’t mean chicken soup. Researchers at Stanford University and the University of California San Francisco have identified a specific protein inside human cells that, when disabled, can stop some of the peskiest viruses in their tracks. The researchers hope that their results, published this week in Nature, may pave the way for a new era in the fight against rhinoviruses (collectively known as “the common cold”) and more serious enteroviruses like polio and those that cause brain inflammation or encephalitis.
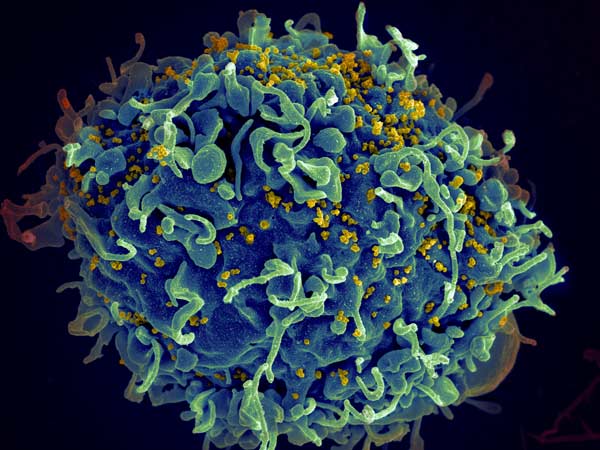
“Our approach is a little bit different than the regular antiviral approach where you directly target viral proteins,” says study senior author Jan E. Carette, a Stanford University microbiologist. Conventional therapies try to destroy viruses by targeting their proteins, which they need to live. But the pathogens need our proteins, too: they proliferate by injecting their DNA into host cells. Different viruses need different proteins to complete this process.
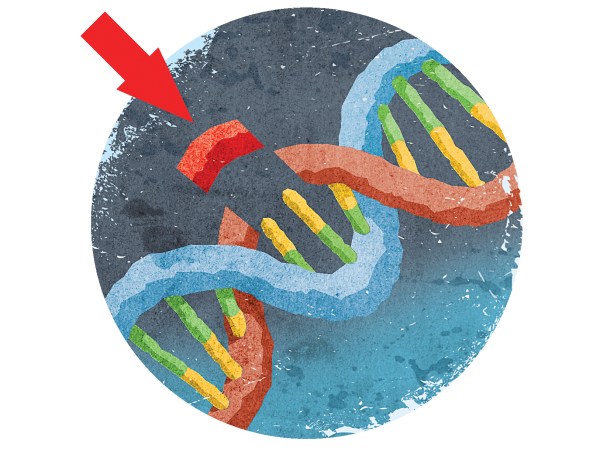
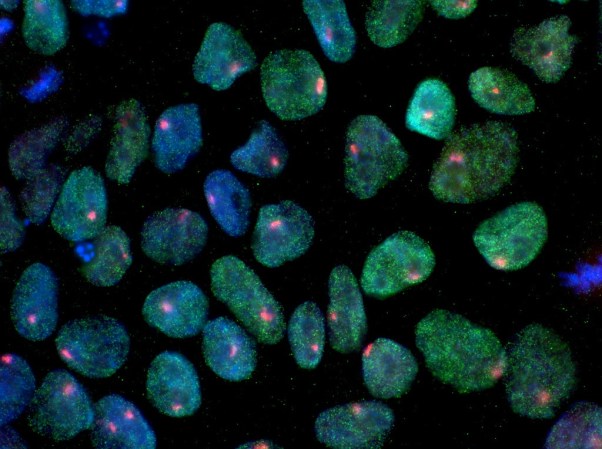
Carette and his colleagues used CRISPR-Cas9 to screen the whole human genome, looking for a protein that all enteroviruses depend on to replicate. Using an existing library of gene knockouts—cells where one gene is made inoperative—they grew a culture featuring knockouts on different genes in different cells, covering all 20,000 genes found in humans. They then infected the culture with a rhinovirus and another type of enterovirus, letting the pathogens and cells battle it out. A few cells made it and kept replicating, but one successful type caught their attention: the gene made inoperative in it (SETD3) wasn’t known to be involved in viral replication, but the viruses couldn’t replicate in cells that didn’t have the protein SETD3 codes for.
The researchers made a separate colony of cells with SETD3 knocked out and threw a multiple types of enterovirus in, including rhinovirus. But “knockout makes it completely resistant to viral infection,” says Carette. The viruses simply couldn’t make more of themselves. The hope is that inhibiting the protein could treat a diverse group of viruses, and would be harder for pathogens to develop immunity to than methods that attack the viruses themselves.
This discovery, like most, raises at least as many questions as it answers. “It’s a beautiful piece of science,” says Ann C. Palmenberg, a University of Wisconsin, Madison biochemist and enterovirus expert who was not involved with the research. But “don’t throw away your chicken soup just yet,” she says. Until Carette’s team is able to figure out how and why this specific protein is so important to enterovirus replication, she says there’s no way to know what treatments it may or may not lead to. “Getting from where they are to where they would like to be is another 20 years of work,” she says.
That’s work the team wants to do. Unlike human cells grown in the lab, exposing actual humans to permanent full-body CRISPR changes is not a good or feasible idea (and would certainly be overkill for curing a minor bug). The goal would be “to find a chemical that can inactivate this protein and might protect you against infection by these enteroviruses,” Carette says. But until they figure out why the absence of this protein stops enteroviruses in their tracks, Palmenberg says, drug development can’t go forward.
Currently, SETD3 is a mystery, and even the potential impacts of a knockout are far from clear. As part of the work, the team raised mice with inhibited SETD3 genes, and they were able to reach adulthood with no apparent problems—and with a resistance to infection by enteroviruses. But there’s still a lot to figure out about how a drug-induced protein knockout in humans would work, or what side effects it might have.
“We discovered a drug target in the cell,” says Carette. But that’s just the start. Even if this study really does mark the beginning of the end of our battle with the common cold, any therapy based on the discovery would need years of development before large-scale human trials could begin. Keep your chicken soup and boxes of tissues handy—the sniffles are here to stay for a long while yet.