Medical device makers have been trying to come up with a better way for diabetics to measure their blood glucose levels for decades, but while a handful of promising methods have enjoyed measured success, the finger-pricking, blood-drawing glucose meter is still the most common tool for everyday use. But a new development in an old research pursuit at MIT may finally provide diabetics with a painless means of checking their sugar, by simply shining a light on their skin.
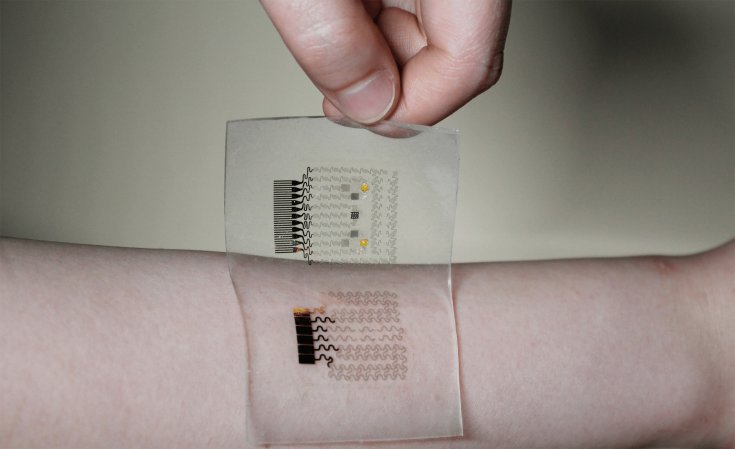
Researchers at MIT’s Spectroscopy Lab have been working for more than a decade on a method of using Raman spectroscopy to measure glucose levels. That approach involves shining near-infrared light on the patient’s arm or finger and using the ensuing vibrations put off by the chemical bonds in various molecules in the skin to measure the amount of glucose present.
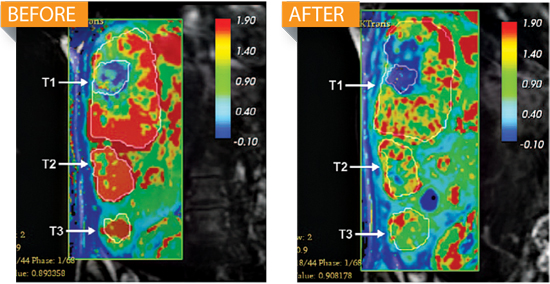
The method works well, but the IR light can only penetrate about half a millimeter below the skin. That means glucose readings are actually measuring the amount of sugar in the interstitial fluid surrounding skin cells rather than the bloodstream. To overcome this problem, the team developed an algorithm that relates the two different glucose concentrations so the device can extrapolate the amount of glucose in the bloodstream from the amount of glucose in the skin.
But another problem persisted: directly after eating, a patient’s blood glucose soars. His or her interstitial fluid levels might take up to ten minutes to catch up, resulting in a faulty reading. To deal with this lag, the team developed another method of correcting for the difference between blood glucose and skin glucose levels called Dynamic Concentration Correction (DCC). By adding the rate at which glucose diffuses from blood to skin into the larger equation, they found they were able to improve the accuracy of their readings by up to 30 percent in the best cases and 15 percent on average.
Raman spectroscopy still isn’t perfect, but the breakthrough is a pretty big step toward solving a problem that has persisted for years with only measured progress. The MIT team plans to get a clinical trial underway on healthy patients in the fall to see if DCC can stand up in a more real-world setting. If it does, those finger-pricking meters could become a thing of the past.