Many Promising Embryonic Stem Cell Therapies Ensnared In Legal Loophole
Rules from two U.S. federal agencies, the National Institutes of Health and the Food and Drug Administration, have created a strange impasse.
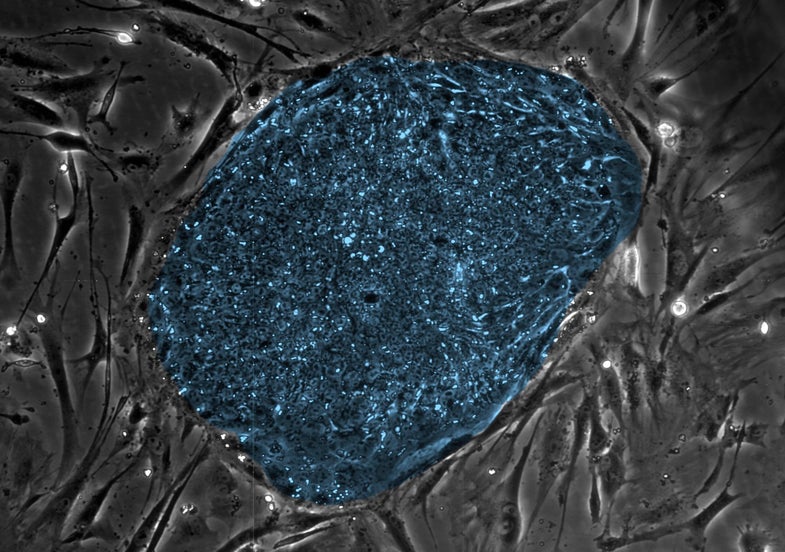
Hey, isn’t it great that university scientists are working on making embryonic stem cell therapies? They’ve done some especially promising work in treating certain causes of blindness, including age-related macular degeneration. But now a strange but serious roadblock has come up. Because of certain federal rules, the majority of embryonic stem cell therapies being studied in universities actually aren’t eligible to become sellable treatments, the journal Cell Stem Cell reports.
Universities usually do research on U.S. National Institutes of Health-registered embryonic stem cells. However, the NIH’s rules don’t match up with rules from the U.S. Food and Drug Administration, which would have to approve any embryonic stem cell-based therapy for use the U.S. So these university-created treatments technically aren’t allowed to move past the research stage. What a dilemma!
Historically, the FDA has allowed clinical trials of therapies created from NIH-registered embryonic stem cells, which suggests the administration knows what’s going on and is willing to move stem cell therapies along. So maybe the rules will change in the future. For now, however, they’re at an impasse.
This is a new problem, brought on by the speed of the advancement of embryonic stem cell research.
This is a pretty new problem, brought on by the speed of the advancement of embryonic stem cell research. The NIH-FDA mismatch wasn’t a big deal in the early days of the field. “I just don’t think people think about [commercialization] while they’re doing research until, ‘Whoa, we could be close,'” Joy Cavagnaro, the president of a drug development consulting firm called Access Bio, told the magazine The Scientist. “And now it’s an issue.”
Why does this weird mismatch exist in the first place? In brief, it’s because the NIH’s and FDA’s jobs are slightly different.
The NIH’s rules were set up to ensure scientists obtained embryonic stem cells ethically. They require that the cells come only from embryos created for in vitro fertilization, a fertility treatment during which infertile couples create a bunch of embryos in lab. Usually couples don’t use all of their embryos, so they are able to donate the extras to research, if they like. The NIH requires registered embryonic stem cells come with a signed form from the parents saying they wanted to donate their embryos to research. Any scientists that don’t use NIH-registered embryonic stem cells can’t get NIH funding, which would be a huge loss for universities and other nonprofits.
The job of the FDA, on the other hand, is to ensure prescription medicines in the U.S. are safe and effective. That means it wants all embryonic stem cell therapies to come from embryos whose parents have been tested for a battery of diseases, including HIV, hepatitis B and C, and prion diseases, a family of infections that are related to mad cow disease. For the majority of NIH-registered embryos, that never happened.
The best solution might be retroactive testing of the embryos for diseases. So far, the FDA hasn’t said that retroactive testing is an acceptable replacement for parent testing, Cell Stem Cell reports, so things are still in limbo.