When Kira Walker was born, on June 13, 2013, her parents and doctors knew she might have health issues. Her mother, a recovering heroin addict, had taken methadone to manage her addiction throughout the pregnancy. Kira was admitted to the neonatal intensive care unit (NICU) at the Research Medical Center in Kansas City, Missouri, where she was born, so that doctors could watch for withdrawal symptoms. That’s why they happened to notice she had a different and equally serious problem: abnormally low blood sugar.
At first, Kira’s doctors could control her blood sugar with cortisol, and she was allowed to go home. But at her one-month checkup, her blood sugar was so low that the glucose meter couldn’t initially read it. Kira was admitted to nearby Children’s Mercy Hospital in Kansas City, where doctors ran a slew of tests to determine the cause. No luck. With her blood sugar dropping precipitously, Kira would go limp at times. And every day that the level continued to yo-yo brought her closer to brain damage. No one knew what to do.
Kira was exceptionally lucky to have landed at Children’s Mercy. The hospital is one of a handful in the U.S. that can sequence babies’ whole genomes in just a few days—a feat that two decades ago would have taken 10 years. By sequencing her genome, doctors might uncover a genetic clue to her condition and suggest a therapy. They took samples of blood from Kira and her parents on a Thursday and sent them to the hospital’s lab for sequencing. By Sunday evening, they had the results.
Kira, they learned, had inherited a mutated copy of a gene known as ABCC8 from her father; the other copy had randomly mutated in some of her pancreatic cells as she developed in utero. The mutation caused the affected cells to constantly secrete insulin, the hormone that removes sugar from blood. Luckily, about 60 percent of her pancreatic cells remained healthy, so doctors could remove the rogue ones and leave the rest of her organ intact. (If more of her pancreas had been affected, she might have become diabetic.) Children’s Mercy flew Kira and her family to the Children’s Hospital of Philadelphia, where surgeons specialize in treating the disease. On August 30, two-month-old Kira went into surgery. When she came out three hours later, she was cured.
Doctors at Children’s Mercy estimate that as many as one third of all newborns admitted to NICUs in the U.S. suffer from genetic diseases like Kira’s—conditions caused by single-gene mutations that are difficult, if not impossible, to diagnose with standard clinical tests. Worse, patients often have to wait four to six weeks for results, time that many sick babies do not have. Certainly, some of the more common genetic diseases are well-known and easy to identify—I’m pregnant, and early in my first trimester I took a blood test to determine if I harbored mutations associated with more than 100 of them. (I don’t.) But there are now more than 4,000 known genetic diseases caused by single-gene mutations.
By analyzing a baby’s genome, doctors can look at all possible genetic causes of a condition simultaneously, and in the span of just 50 hours, says Stephen Kings-more, director of the Center for Pediatric Genomic Medicine at Children’s Mercy Hospital. Over the past couple of years, Kings-more led a small pilot project to sequence the genomes of 36 infants, including Kira’s. For a clinical trial funded by the National Institutes of Health (NIH), he says, the hospital is now beginning to sequence the genomes of 1,000 more.
This capability could change neonatal medicine forever. The clinical trial at Children’s Mercy, along with three other trials soon to start at different institutions, will elucidate the benefits and drawbacks of such knowledge. Other doctors, meanwhile, are developing reproductive technologies that could prevent debilitating conditions entirely, giving parents-to-be a virtual guarantee that their babies will be healthy. These technologies, while exciting, raise tough questions too—about newborn and fetal rights, the possibility of genetic discrimination, and where, ultimately, we should draw the line when it comes to genetic tinkering. Few would argue against preventing disease—but what happens when parents can design aesthetically beautiful, genetically superior babies?
* * *
In April 2003, after 13 years of hair-pulling work and nearly $3 billion in costs, scientists with the Human Genome Project announced that they had finished sequencing the first complete human genome. Many doctors believed the information would revolutionize medicine overnight—that with humanity’s full genetic code mapped out, scientists would be able to identify the cause of most conditions and then engineer ways to fix them. “People thought that we’d have medical care like Star Trek,” says Josh Petrikin, a neonatologist at Children’s Mercy Hospital.
That’s not what happened. For one, the sequencing itself—deciphering the exact order of three billion tiny little letters, or nucleotides—was time-consuming and expensive. It also proved exceptionally difficult to interpret meaningfully. It was like trying to read a book written by Martians, if the language was not only totally unfamiliar but also riddled with enormously complicated and inconsistent rules. To make matters worse, scientists soon realized that most diseases weren’t caused by mutations in single genes; many were either caused by mutations in multiple genes or none at all.
Doctors estimate that as many as one third of all newborns admitted to neonatal intensive care units in the U.S. suffer from genetic diseases.
Now, 11 years later, the diagnostic and therapeutic promise of whole-genome sequencing is finally blossoming—at least for babies. Most diseases that afflict adults are caused by a complex array of genetic and environmental factors. But genetic diseases are the leading cause of death in infants, and many are caused by a single-gene mutation. These “monogenic” diseases include well-known conditions such as cystic fibrosis, sickle-cell anemia, and Tay-Sachs disease, as well as thousands of exceedingly rare illnesses that each afflict no more than a handful to a few hundred individuals in the world. This uniqueness makes them very difficult to diagnose clinically, but because they are relatively simple genetically, they are, in theory, easy to diagnose with gene sequencing. Additionally, the cost and time involved has dropped exponentially in the past decade, and bioinformatics software has become much better at matching genetic mutations to known symptoms and conditions. It makes sense, then, that sick babies should be among the first to benefit from the technology.
Four years ago, geneticist Stephen Kingsmore, then CEO of the National Center for Genome Resources in Santa Fe, New Mexico, had this epiphany. His team of researchers had been sequencing the genomes of cocoa and rice. “We realized that what we were doing in plants was going to hit medicine,” he says, “so we decided to try to surf that big wave.” A native of Northern Ireland with a dry sense of humor, Kingsmore moved from Santa Fe to Kansas City to open the Center for Pediatric Genomic Medicine. Soon after, he heard that the biotechnology company Illumina was looking for a hospital to beta-test its newest and fastest sequencer, the HiSeq 2500. “They said, ‘We’ve got this new sequencer; what do we do with this?’ ” Kingsmore recalls. “We said, ‘We know exactly what to do with that. Let’s use it in critically ill babies, as most babies die before they get diagnosed.’ ”
Since the hospital’s pilot project began, in November 2011, doctors have correctly diagnosed 18 out of 36 mysteriously sick babies—most of whom would have otherwise waited months for a diagnosis, if they survived that long. When I walked through the Children’s Mercy NICU with Petrikin and Howard Kilbride, the hospital’s director of neonatology, we encountered three-month-old Eliana Lewis sleeping in her father’s arms. Eliana was born on New Year’s Eve 2013, and soon after she got home, she began suffering brain seizures every couple of minutes. They couldn’t be stopped with standard medications, so doctors kept her heavily sedated. Whole–genome sequencing at Children’s Mercy eventually diagnosed Eliana with Ohtahara syndrome, caused by a mutation in the gene SCN2A and sometimes controllable with a low-sugar diet. Eliana started the diet in March, and her seizures improved dramatically: She is no longer as sedated or on a ventilator. “We’re really starting to see her personality now,” her mother, Michelle Lewis, told me. “She’s starting to have periods of being awake and alert.”
Even Kingsmore has been shocked by how fruitful the sequencing efforts have proved to be. “Never did we expect what we’re finding—that the majority of the kids we’re testing would yield a diagnosis. That’s crazy,” he says, especially considering that scientists still don’t understand much of the human genome. Including children that weren’t part of the pilot project, he says, “We have dozens and dozens of stories of kids whose lives have been saved or transformed, their families given hope, because of this inexpensive genetic test.”
Of course, not every story has had a happy ending. Eliana’s prognosis, for instance, isn’t great: Even when babies with Ohtahara syndrome survive past infancy, they are often severely intellectually disabled. And for some, a diagnosis is a dead end, with no known treatments; only seven of the infants in the pilot project had a treatable diagnosis. “Those happen, and those are sad, but I feel like it’s still doing some good to get a diagnosis—decreasing suffering, giving the family an answer,” Petrikin says. Lewis agrees. “Obviously our diagnosis is not the greatest thing in the world,” she says, “but we know what we’re fighting against, and that allows us to process things.”
“People are going to be able to say,’I want my baby to be a girl, I want her not to carry the breast cancer gene, and I want her to have blue eyes.'”
With the NIH trial, Children’s Mercy hopes to provide even more families with the answers and treatments they need. In the NICU, I stopped to peek at a three-week-old baby named Xavier in an incubator. He had been born with his bowels outside his body, a condition that is becoming more common and could have a genetic component. His doctors had attempted multiple surgeries to move his intestines inside, but his body had rejected them each time. Could sequencing pinpoint the cause of his birth defect and help his doctors understand why his body reacted the way it did? Perhaps. We passed another baby on a ventilator, tightly wrapped in a blanket, who had problems taking his first breaths outside the womb and had gone on to develop pulmonary hypertension. Babies with this condition respond differently to treatments, possibly because the symptoms have different underlying genetic causes. Sequencing could potentially get them the right care faster. “Ideally, we’d like to personalize what we’re doing rather than treat everybody the same,” Kilbride says. “A blood test focusing you and maybe even giving you a diagnosis in a few days? I mean, that would be revolutionary.”
* * *
When Alexis Sturgeon’s now 27-year-old brother was 15, he started vomiting incessantly. Doctors first thought he had the flu, but he didn’t improve. Several hospital visits and many tests later, he was diagnosed with late-onset ornithine transcarbamylase (OTC) deficiency, a rare disorder that can be caused by a mutation in the OTC gene. Normally, OTC makes a protein that helps to process nitrogen. Without a functioning copy of the gene, the body builds up toxic ammonia. Since his diagnosis, Sturgeon’s brother has had to take drugs—sometimes up to 100 pills a day—to supply enough of the missing protein to keep him healthy.

The OTC gene is located on the X chromosome, which means that men, who carry one X and one Y chromosome, develop the disorder if they inherit the mutation. Women, on the other hand, are more often asymptomatic carriers, because even if they inherit one defective gene, the copy on their second X chromosome is typically able to produce sufficient quantities of the protein to keep them healthy.
Alexis Sturgeon felt fine, but she decided to get her own OTC genes tested anyway. She was indeed an asymptomatic carrier of the disease. Although she would likely be healthy for life, Sturgeon hoped to have children, and she didn’t want to pass the mutation on to them. If she had girls, they might not get sick, but they would have a 50 percent chance of inheriting one mutated gene and carrying the legacy of the disease to future generations. If she had boys, they would have a 50 percent chance of inheriting her mutated gene and developing the full-blown disorder. Sturgeon wanted to know: Was there anything she could do to ensure that she would have a healthy baby?
Geneticists like Santiago Munné have dedicated their lives to answering these kinds of questions. In the early 1990s, after he’d finished his Ph.D. in genetics, Munné realized that the people who could potentially benefit the most from improvements in genetic technology were women hoping to conceive. Doctors typically told women like Sturgeon that they had no choice but to roll the dice and hope their children beat the odds. “Usually, we were just giving people bad news,” he says.
So Munné went to work to develop better alternatives. In 1993, while collaborating with Jacques Cohen at Cornell University Medical College, he developed the first test to screen in vitro fertilization (IVF) embryos for chromosomal defects, such as those that cause Down syndrome. Fertility doctors could use the test to select only healthy embryos for implantation, thereby eliminating the risk for such disorders.
In 2001, Munné co-founded New Jersey–based Reprogenetics, one of a handful of biotech companies dedicated to developing new reproductive technologies. Munné’s team has drastically improved its chromosome test in the past four years so that it can detect more conditions. The company has also developed preimplantation genetic diagnosis tests that can screen IVF embryos for single-gene disorders such as OTC deficiency.
“I’m very grateful that there are people out here who are smart enough to figure all this out.”
When Sturgeon was ready to have kids, her doctor told her about the Reprogenetics test, and she immediately agreed to undergo IVF so she could use it. First her doctor took DNA swabs from Sturgeon’s and her husband’s cheeks to map their genes. She was also put on fertility drugs for several weeks. Then her doctor harvested seven of Sturgeon’s eggs, fertilized them with her husband’s sperm, extracted a single cell from each embryo when they were three days old, and sent the cells to Reprogenetics for testing. The next day, the company was able to tell her doctor which embryos carried the OTC mutation and which did not. On August 11, 2013, Sturgeon gave birth to a baby girl, Audrey, who has two functioning copies of the OTC gene. “I’m very grateful that there are people out here who are smart enough to figure all this out—to be able to give people who have these sorts of disorders a chance of having a healthy child,” she says.
Munné says that screening for single-gene disorders is just the beginning. His company has also developed tests that can screen embryos for mutations in the BRCA1 and BRCA2 genes, which increase the risk of breast cancer. He hopes to soon be able to screen embryos for gene defects linked to autism, schizophrenia, and Alzheimer’s too. And then there is the near-reality of whole-genome embryonic screening. While single-gene tests like the one used to screen Sturgeon’s embryos work well when a familial genetic condition is known, many prospective parents are disease carriers without realizing it. Plus, Munné’s research has shown that during conception, as many as 3,000 de novo mutations can arise that no one would be able to predict.
On May 18, 2014, a baby was born whose genome had been sequenced prior to IVF implantation to check for potential genetic mutations—a global first. Although it was just a proof-of-concept run, Munné says that as soon as the cost for whole genome sequencing drops below $1,000—which researchers believe could happen this year—it will be feasible for Reprogenetics to offer preimplantation genome sequencing to families who want it.
* * *
Genes, of course, predict far more than disease. So if doctors can create healthy babies, what’s stopping them from making babies with other sought-after characteristics? Not much, some say. “Once you’re able to look at and identify chromosomes in embryos, then you can study everything in that embryo—and the term everything keeps expanding,” explains fertility doctor Jeffrey Steinberg, director of The Fertility Institutes. “People are going to be able to come in and say, ‘I don’t want my baby to have Down syndrome, I want my baby to be a girl, I want my baby not to carry the breast-cancer gene, and I want my baby to have blue eyes.’ ”
The baby-girl part is already a reality. Although 36 countries have outlawed sex selection, the practice is legal and booming in the U.S., despite the fact that the procedure can cost upwards of $18,000. Out of 415 reproductive clinics surveyed in 2006, nearly half said they were offering preimplantation genetic diagnosis for “nonmedical” reasons, and the percentage has gone up since. Steinberg, for instance, says that 90 percent of the couples who come to his clinic want to choose their babies’ sex.
Most American families who undergo sex selection do it for family balancing or health reasons. After using IVF to conceive two boys, now ages four and three, Shannon Twisler and her husband, who reside in Phillipsburg, New Jersey, decided to try for a girl. Since she was going to undergo IVF again anyway (the couple could not conceive naturally), why not have the doctor implant a female embryo? “It was kind of a no-brainer for us,” Twisler says. “I have one older sister who has three boys, and she really wanted a girl, and my mom had four girls but wanted a boy. It seemed like it was a pattern in my family to have one gender or another.” It was a pattern she’d hoped to buck with technology—and she did. Between the embryos she had frozen from her earlier IVF cycles and the third round of IVF she underwent last summer, she and her husband produced a single female embryo, which her doctor implanted in January 2014. She is due with a baby girl in October.

But sex selection is only the beginning. Steinberg says he also knows how to select for babies with blue eyes, by looking for a variant in that gene that control the amount of pigment in the stroma of the iris. “If you have a lot of pigment, you make brown eyes,” he explains, “and if you have no pigment, you make blue eyes. In between, you make green or hazel.” In 2009, Steinberg announced that he was going to offer eye-color selection in his clinic. “It set off a firestorm—we got a huge number of people super-interested in it, and we got a huge number of people threatening us.” He says he even received a call from the Vatican, whose scientists asked him to reconsider offering the service. He complied because, as he puts it, “technology seemed to be moving faster than society’s ability to deal with it.”
But Steinberg is confident that public opinion is changing. “A lot of the social criticism has settled down,” he says. “Twenty years ago, people thought IVF was going to produce zombies, but now you go to a party and half the people there are IVF babies. Selecting for eye color will become a reality in the next five years.” Hair-color selection isn’t far off, either, he adds: In June, Stanford University scientists announced they had identified a gene variant that contributes to blondness in human hair.
Others disagree that these technologies are mature. “I don’t think it’s that simple, I really don’t,” says Richard Paulson, chief of reproductive endocrinology and fertility at the University of Southern California’s Keck School of Medicine. “I think that people who are peddling this, who are advertising on their websites that the capability [for eye-color selection] exists, are not being intellectually honest.” Steinberg acknowledges that his eye-color-selection method is only 90 to 94 percent accurate; he is raising money for additional research to increase the accuracy to 99 percent, at which point he says he will begin offering the service.
Choosing a child’s features is, of course, controversial for a number of reasons that have nothing to do with technology. The American Congress of Obstetricians and Gynecologists worries that sex selection reinforces biases against women. (Interestingly, though, more than half of parents who use sex selection in the U.S. do it to have baby girls.) There’s also the question of what happens to the embryos that parents deem unworthy. Will thousands of brown-eyed embryos suddenly end up in the trash? Twisler plans to donate her extra frozen embryos to other families, but couples undergoing sex selection have the option of throwing away unused embryos. Then there is the “slippery slope” argument—that once we start selecting for sex, eye color, and hair color, what’s to stop wealthy parents from engineering smarter, more athletic, and more conventionally beautiful babies too? This is where visions of Gattaca come in: One can imagine a world where designer kids of well-to-do parents outcompete their genetically inferior, naturally conceived counterparts. Genetic discrimination becomes rampant, and wars start.
“Selecting for eye color will become a reality in the next five years.”
But the science of Gattaca is still a long way off. For one thing, traits like IQ, height, and beauty are enormously complex. Scientists still haven’t identified all of the genes involved, so there is no known “recipe” for an IQ of 140 or a symmetrical face. And the best that fertility clinics can do today is choose among embryos that have been produced naturally from parents’ genetic material. There’s virtually no chance that doctors will be able to implant a genius baby from two parents with average IQs. That would require genetic engineering—tinkering with embryonic genes—which nobody yet knows how to do. “People seem to think there’s a menu of 1,000 different characteristics, and parents will be able to choose what they want,” Paulson says. “It doesn’t work like that.”
As a mother to a three-year-old, with another baby on the way, I can’t imagine wanting that anyway. Part of what makes me so excited to meet my baby girl is knowing that she is half mine, half my husband’s—a natural genetic blend of the two of us. Would it be nice if I could be sure that she hadn’t inherited my bad back or my husband’s propensity for gastric reflux? Sure. So selecting embryos for medical reasons makes sense to me. I can also understand the desire to want a balanced family; I was thrilled when I found out we would have one of each. But manipulating my daughter’s genes so that she looks more like Charlize Theron? Doesn’t have the same appeal. I’m not going to love my little girl any less if she has brown eyes rather than blue, and I can’t imagine she will suffer terribly for it either.
One thing is for sure: Genetic research is advancing rapidly, so it’s conceivable that our children or grandchildren will live in a world in which they can “design” their babies, at least to a degree. The question, really, is whether the values of future generations-—those whose lives have been shaped by this newfound knowledge-—will embrace such a future or fight against it.
How to Solve a Mystery Baby
Doctors at the Center for Pediatric Genomic Medicine at Children’s Mercy Hospital in Kansas City, Missouri, worked with biotechnology company Illumina to develop a protocol for sequencing the full genomes of newborns. It enables them to home in on the cause of rare diseases in just 50 hours.
Step 1: Eliana Lewis was born on New Year’s Eve 2013, and she had problems almost immediately: fluctuating blood sugar, and seizures every few minutes. When drugs didn’t help, doctors took blood samples from both Eliana and her parents and sent them to the hospital’s lab.
Step 2: Technicians isolated DNA from the blood, copied it millions of times, and used ultrasound to chop it into easy-to-read pieces. They then loaded a chip containing the DNA samples into Illumina’s HiSeq 2500 sequencer, which reads all the fragments in 26 hours.
Step 3: A supercomputer took that information and reordered it by aligning the genetic fragments with those in a reference genome. Then the computer searched for differences among the three samples and the reference; there can be five million, and most are probably harmless.
Step 4: Bioinformatics software determined that Eliana had a mutation in the SCN2A gene that neither of her parents had. (It must have spontaneously occurred in the sperm or egg before she was conceived.) The mutation suggested she had Ohtahara syndrome, a rare form of pediatric epilepsy.
Step 5: Doctors tried new medications in light of Eliana’s diagnosis. By March, her health had improved enough to start her on a low-carbohydrate diet that has been successful in managing Ohta-hara syndrome. In May, she was released from the hospital with her seizures under control.
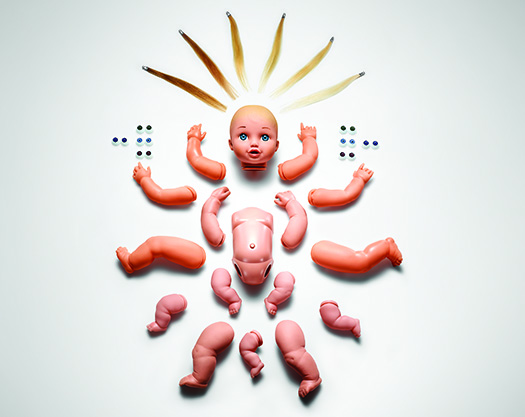
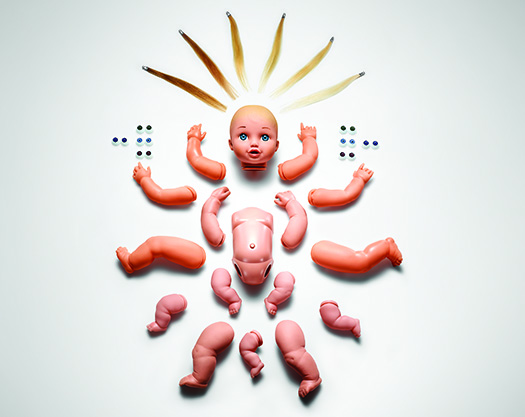
A Healthy Baby from Scratch
The Food and Drug Administration is weighing whether to approve U.S. clinical trials for another cutting-edge technique: three-parent in vitro fertilization.
Parents-to-be who want to conceive a baby with IVF can use genetic testing to choose healthy embryos. But hopeful moms with rare disorders affecting mitochondria, the energy-producing organelles that sit outside a cell’s nucleus, don’t have that option: Their diseased mitochondria almost always get passed down, producing a devastating illness. One possible solution is to create a baby from the genetic material of three people.
The procedure, called oocyte modification, involves replacing the nucleus of a donor woman’s egg with that of the intended mother’s, either before or after the nucleus of the mother’s egg has been fertilized with the father’s sperm. The new hybrid embryo contains the nuclear DNA of both mom and dad and the healthy mitochondria of the donor.
“This technique is extremely exciting because it completely eliminates a fatal, incurable genetic condition from future generations, allowing women who carry this disease to have their own genetic children free from disease,” says Susan L. Solomon, CEO and cofounder of the New York Stem Cell Foundation, whose scientists have conducted some of the research. But like many other reproductive technologies for shaping a baby’s genetic future, this one has inspired controversy.
_This article originally appeared in the August 2014 issue of _Popular Science.
