A device the size of an espresso machine quietly whirs to life. The contraption isn’t filled with fresh, pungent grounds but, instead, spoonfuls of opaque, sterile goo. Its robotic arm moves briskly: It hovers, lowers, and then repositions a pair of syringes over six petri dishes. In short, rapid-fire bursts, they extrude the milky paste. Soon, three little hexagons form in each dish. After a few minutes, the hexagons grow to honeycomb structures the size of fingernails. No one here is getting a latte anytime soon.
The honeycombs are human livers, says Sharon Presnell, chief technology officer of Organovo—or at least the foundations of them. The tiny masterpieces of biomedical engineering are nearly identical to tissue samples from real human livers, and they are constructed from actual human cells. But instead of growing them, scientists in the gleaming, 15,000-square-foot headquarters of Organovo print them, just as they would a document. Or, more accurately, just as they’d print a scale model.
In two decades, 3-D printing has grown from a niche manufacturing process to a $2.7-billion industry, responsible for the fabrication of all sorts of things: toys, wristwatches, airplane parts, food. Now scientists are working to apply similar 3-D–printing technology to the field of medicine, accelerating an equally dramatic change. But it’s much different, and much easier, to print with plastic, metal, or chocolate than to print with living cells.
“It’s been a tough slog in some ways, but we’re at a tipping point,” says Dean Kamen, founder of DEKA Research & Development, who holds more than 440 patents, many of them for medical devices. In labs around the world, bioengineers have begun to print prototype body parts: heart valves, ears, artificial bone, joints, menisci, vascular tubes, and skin grafts. “If you have a compass and a straight edge, everything you draw is a box or a circle,” Kamen says. “When you get better tools, you start thinking in different ways. We now have the ability to play at a level we couldn’t play at before.”
From 2008 to 2011, the number of scientific papers referencing bioprinting nearly tripled. Investment in the field has spiked as well. Since 2007, the National Heart, Lung, and Blood Institute of the National Institutes of Health has awarded $600,000 in grants to bioprinting projects. Last year, Organovo, raised $24.7 million in equity.
Three factors are driving the trend: more sophisticated printers, advances in regenerative medicine, and refined CAD software. To print the liver tissue at Organovo, Vivian Gorgen, a 25-year-old systems engineer, simply had to click “run program” with a mouse. Honeycomb-shaped liver tissue is a long way from a fully functioning organ, but it is a tangible step in that direction. “Getting to a whole organ-in-a-box that’s plug-and-play and ready to go, I believe that could happen in my lifetime,” says Presnell. “I cannot wait to see what people like Vivian do. The potential is just out of this world.”
* * *
The very first bioprinters weren’t expensive or fancy. They resembled cheap desktop printers because, in fact, that’s what they were. In 2000, bioengineer Thomas Boland, the self-described “grandfather of bioprinting,” eyed an old Lexmark printer in his lab at Clemson University. Scientists had already modified inkjet printers to print fragments of DNA, in order to study gene expression. If an inkjet could print genes, Boland thought, perhaps the same hardware could print other biomaterials. After all, the smallest human cells are 10 micrometers, roughly the dimension of standard ink droplets.
Boland emptied the Lexmark’s ink cartridge and filled it with collagen. He then glued a thin, black silicon sheet onto blank paper and fed it into the printer. He opened a Word document on his PC, typed his initials, and hit print. The paper spooled out with “TB” clearly delineated in off-white proteins.

By 2000, Boland and his team had reconfigured a Hewlett-Packard DeskJet 550C to print with E. coli bacteria. Then they graduated to larger mammalian cells, farmed from Chinese hamsters and lab rats. After printing, 90 percent of the cells remained viable, which meant the product was useful, not simply art. In 2003, Boland filed the first patent for printing cells.
While Boland’s lab worked out the problem of bioprinting, other engineers applied 3-D printers to different medical challenges. They printed bone grafts from ceramic, dental crowns from porcelain, hearing aids from acrylic, and prosthetic limbs from polymer. But those engineers had an advantage that Boland and his colleagues did not: They could print in three dimensions rather than just two.
So Boland and other bioprinting pioneers modified their printers. They disabled the paper-feed mechanisms in their inkjets and added an elevator-like platform controlled by stepper motors; the platform could move up or down along the z-axis. Labs could print one layer of cells, lower the platform, and print another layer. Suddenly, bioengineers went from drawing life on a flat canvas to building living sculptures.
“It was like magic,” says James Yoo, a researcher at the Wake Forest Institute for Regenerative Medicine who is developing a portable printer to graft skin directly onto burn victims. The ability to print cells in three dimensions opened up new applications. “Every wound is different; the depth is different; and they’re very irregular,” Yoo says. “By mapping the area, you can determine how many cell layers are needed for the subdermal tissue, as well as the epithelial area. The advantage of the printer is that you can deliver cells more accurately and precisely.”
Scientists could also print with many types of “ink.” Cornell engineer Hod Lipson, co-author of Fabricated: The New World of 3D Printing, prototyped another kind of tissue: cartilage. “The spatial control over the placement of cells has never been possible to this degree,” he says. “That opens up multiple dimensions of possibilities.” Lipson and his colleagues decided to print a meniscus, the C-shaped piece of cartilage that cushions the knee and other joints. The team used CT scans to create a CAD file of a sheep’s meniscus and extracted cells from the sheep to print an identical one.

Although Lipson’s first meniscus looked promising, when he showed it to knee-replacement surgeons, they deemed it too weak to withstand the body’s routine abuse. “As somewhat of an outsider coming in [to biology], my impression was ‘Okay, I’m gonna put the cells in the right place, incubate it for a while, and we’re gonna have our meniscus,’ ” Lipson says. “There is more to making a meniscus than just putting the cells there. Real menisci are actually pounded every day, all the time, and they shape up and become stiff. So the pounding that’s in their environment is actually very much a part of their growth.”
Suddenly, bioengineers went from drawing life on a flat canvas to building living sculptures.
A printer that can dispense the right ink, in other words, is only the first step. Cells have specific requirements, depending on the tissue they’re destined to become. In the case of a meniscus, it might mean developing a bioreactor that can approximate pounding or use heat, light, or auditory pulses to stress the tissue into formation. “For some tissues, even the simple ones, we don’t even know exactly what it takes to make the tissue behave like a real tissue,” says Lipson. “You can put the cells of a heart tissue in the right place together, but where’s the start button?”
* * *
Most organs are highly sophisticated structures with dozens of cell types and complex vasculatures evolved to do very specific jobs. The liver alone performs more than 500 functions. Like machines, bodies wear out and break down over time, sometimes unexpectedly. Even when transplants are feasible, donated organs can’t keep pace with demand. So as mechanical engineers began to build early 3-D printers, tissue engineers tried growing replacement organs in a lab.
They started by pipetting cells into petri dishes by hand. Then, led by Anthony Atala at the Wake Forest Institute for Regenerative Medicine, researchers began to seed those cells onto artificial scaffolds. Made from biodegradable polymers or collagen, the scaffolds provide a temporary matrix for cells to cling to until they’re robust enough to stand alone. The system worked beautifully: Atala successfully implanted the first lab-grown organs—bladders—into seven patients at Boston Children’s Hospital between 1999 and 2001.
Researchers soon adopted 3-D printers to make scaffolds more precisely. But manually placing the cells onto them remained a time-consuming and arduous process. Printed bladders can be made with just two cell types; kidneys, for example, consist of 30. “When you try to engineer more complex tissues, there’s no way you can manually place different cell types into different locations that can replicate the native tissue structures,” says Yoo. “Hands are not the optimal method for delivering cells.”

At Wake Forest, Yoo’s and Atala’s teams built custom bioprinters that are faster than modified inkjets and can print with many more cell types—including stem cells, muscle cells, and vascular cells. They also designed one printer to create both the synthetic scaffold and tissue in one fell swoop; they’re now using it to produce intricate ears, noses, and bones.
Scaffolds provide tissues with mechanical stability, and they can be used to deliver genes and growth factors to developing cells. But, as in the case of polymers, they can introduce foreign materials into the body and cause inflammation. Cell types also respond differently to certain scaffold materials, and so the more complex the organ, the more complicated the necessary framework—and the more difficult to predict how the cells will migrate around it. As a result, not everyone believes scaffolds are necessary, including Gabor Forgacs, Organovo’s co-founder and a biological physicist at the University of Missouri.
Forgacs’s plan is to print an organ composed entirely of living human tissue and let it assemble itself. “The magic,” he says, “happens after printing has taken place.” Therein lies the biggest misconception about bioprinting: What most people think of as the finished product—the newly printed cellular material—isn’t finished at all.
Once researchers scale up the vascular system, printed organs will become only a matter of time.
At Missouri, Forgacs studied morphogenesis, the process that determines how cells form organs during embryonic development. By arranging cellular aggregates—tiny spheres containing thousands of cells—into a circle, his lab could watch them fuse and form new structures. The aggregates accomplish this by working together. A molecule on one cell causes a receptor protein on the cell membrane to change shape, tugging on the cytoskeleton of a second cell. A cascade of communication ensues, eventually reaching the nucleus and triggering a change in gene expression.
A grant from the National Science Foundation enabled Forgacs and his team to experiment with bioprinters instead of laying down aggregates by hand, and the technology transformed their research. “What had taken us days, we could do in maybe two minutes,” he says. Using a bioprinter, Forgacs proved that aggregates containing different cell types also fuse, without any human intervention or environmental cues.
Tissue engineers shouldn’t place cells where they’d be in a finished organ, Forgacs says; they should arrange cells based on where they need to be to start forming an organ, as in an embryo. “The cells know what to do because they’ve been doing this for millions of years. They learned the rules of the game during evolution.”
Another key lies in printing cellular aggregates. “You will never build an extended biological structure, a big organ or tissue, by putting down individual cells,” Forgacs says. “A tissue is very well organized, according to very stringent rules, in cellular sets. A half-millimeter aggregate is already a little piece of tissue. Those pieces bind together and exchange information.”

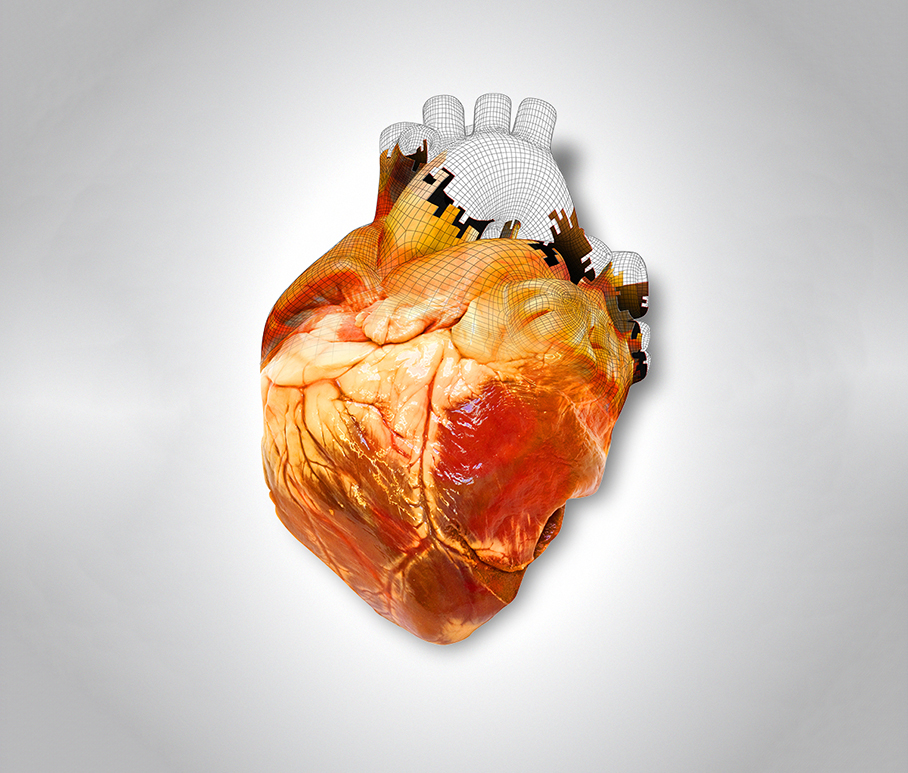
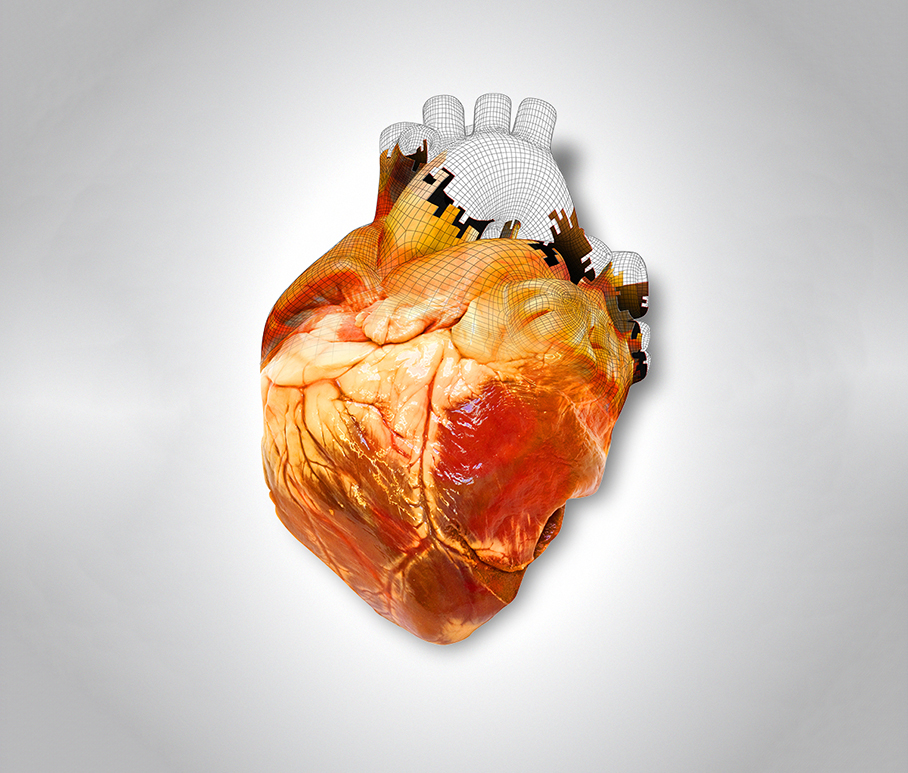
Technologically speaking, it’s already possible to build tissue by stacking piles of cells along the z-axis. In fact, scientists at Organovo did this with cardiac cells; when they fused, they beat in unison, just like a heart. Biologically, however, there’s still a major hurdle: It needs to thrive. An organ requires networks of blood vessels to distribute nutrients and oxygen. Without this core function, cells will wither and die.
Organovo’s researchers have made relatively robust vasculature by printing filler, such as hydrogel, among tubes of tissue cells. The filler can later be extracted, leaving empty channels for blood cells. Ibrahim Ozbolat, a mechanical engineer at the University of Iowa, has also developed a bioprinter, which uses multiple arms moving in tandem, to deposit a vascular network and cellular aggregates at the same time.
“The major challenge,” Ozbolat says, “will be creating very small capillaries”—the hairlike blood vessels linking larger vessels to cells. He foresees wrestling with this in two years. Once researchers can scale up the size and complexity of the vascular system, graduating from biological parts and pieces to whole printed organs will become only a matter of time.
* * *
Actor Bruce Willis gazes at visitors from the side of a machine in a 1,500-square-foot clean room at Organovo. Several of the company’s 10 bioprinters have been named and labeled for characters from the 1997 sci-fi film The Fifth Element. Steps from Willis’s “Dallas,” past a half dozen refrigerator-size incubators, sit the bioprinters “Ruby” and “Zorg,” adorned with photos of Chris Tucker and Gary Oldman, respectively.
In the film, set in the 23rd century, an automated pod with two robotic arms uses cells from a severed human hand to print and reanimate an entire woman. Science is a long way from accomplishing anything remotely close to this feat—and it may never get there. But a major milestone would be to develop tools advanced enough to clearly visualize and model the entire process.

What bioprinters so far lack—and what will enable the field’s next wave of breakthroughs—is biologically sophisticated software. With an inanimate object like a coffee mug, a 3-D scanner can create a CAD file in minutes and upload the design to a 3-D printer. There is no medical equivalent.
“An MRI doesn’t tell you where the cells are,” says Lipson. “We’re just completely in the dark in terms of the blueprints. That’s half the puzzle. There’s also no Photoshop—no tools to move cells around. That’s not a coincidence. It’s beyond what most computer software can handle. You can’t have a software model of a liver. It’s more complicated than a model for a jet plane.”
“Instead of printing a test tube out of plastic to do chemistry in, let’s print our test tube out of tissue.”
Sensing an opportunity, Autodesk has teamed with Organovo to develop CAD programs that could be applied to bioprinting. “The areas we explore don’t always have an immediate business case to be made, but they may have one in the coming years,” says Carlos Olguin, head of Autodesk’s Bio/Nano/Programmable Matter Group. “If so, we want to be ready not just to explore but deliver.”
As a first step, Autodesk plans to create a modern cloud-based CAD shell to help streamline the design process. Eventually, its goal is to integrate the math that describes self-assembly and other cellular processes into bioprinting software. In April, Olguin’s team released Project Cyborg, a Web-based platform geared toward nanoscale molecular modeling and simulations for cellular biology. Ultimately, researchers want to be able to design cellular aggregates digitally, press “enter,” and visualize, in seconds, how the structure would change and evolve into a finished living tissue.
“In the very short term, we’re going to dramatically reduce the time it’s going to take them to bioprint,” Olguin says. “But in the mid-term, by removing them from this amazingly tedious work of creating the most basic shapes, we would hope they would then be able to focus on more interesting applications.”

Organovo’s first biological product will be liver tissue for drug testing. Every year, the pharmaceutical industry spends more than $39 billion on R&D. According to the Food and Drug Administration, liver toxicity is the most common reason for a drug to be pulled from clinical trials—as well as from the marketplace after it’s been approved. There’s still no reliable way to evaluate how a drug will affect the human liver before it’s ingested—not even animal trials.
“There are some pretty significant species differences between animals like rats and humans,” says Organovo’s Presnell. “So you can get a lovely answer from a rat that says, ‘Yeah, go forth!’ And in reality, in a human, it would not do well.”
Bioprinters could build organs with tumors so that surgeons could practice.
At Stanford, researchers have tried to get around this problem by breeding mice with livers made up mostly of human cells. A study published in October showed the mice predicted how well a drug for treating hepatitis C would be metabolized by humans. Scientists at MIT have built miniature liver models using micropatterning, the same soft lithography technique used to put copper wires onto computer chips. The problem, says Presnell, is that micropatterned structures are typically only a couple of cell layers thick, which limits the complexity of questions researchers can ask and answer.
Next year, Organovo will begin selling its liver assay—a petri-dish-like well plate containing liver cells arranged in a 3-D structure 200 to 500 microns thick (two to five times as thick as a human hair). The potential market is vast. Every drug taken orally, whether a painkiller, an anti-inflammatory, or a new cancer pill, must pass a liver tox.
“People normally do a reaction, purify the chemicals, take the drug, add it to cells, look at the response, formulate, maybe do animals, and then go to humans,” says Lee Cronin, a University of Glasgow chemist and nanoscientist developing a 3-D printer to manufacture medicine using chemical inks. “Instead of printing a test tube out of plastic to do chemistry in, let’s say we now print our test tube out of tissue, and we do chemistry in the tissue and look at the response in real time. That’s where things get really interesting.”

If bioprinted assays provide pharmaceutical researchers with better, quicker data, the entire drug-discovery process will accelerate. Moreover, they could lessen the need for extensive animal testing.
Ozbolat’s goal, at the University of Iowa, is to print pancreatic tissue for therapy instead. It would be made up of only the endocrine cells capable of producing insulin. Implanted in people, such tissue could regulate blood sugar and treat type 1 diabetes, he says.
Bioprinters could also prove invaluable for medical schools. Students now train on cadavers, but when it comes to procedures like cutting out cancer, nothing matches the real experience. Rather than printing healthy tissue, bioprinters could build organs with tumors or other defects so that surgeons could practice before entering an operating room.
Whole, transplantable organs that function properly will be the ultimate challenge, but also, in the long run, change lives most profoundly. In the U.S., more than 118,000 people are currently on the national donor waiting list, which grows by 300 every month. It’s not just an issue of supply versus demand. The odds of finding a suitable match are low. Bioprinting organs with cells grown from a patient’s own body could eventually help doctors churn out perfect matches at will.
Perhaps, scientists say, bioprinters could even enable bionic organs—body parts that don’t just restore, but extend human ability. To that end, researchers at Princeton University have been experimenting with integrating electronics into bioprinting. Earlier this year, they created a matrix of hydrogel and bovine cells in the shape of an ear, incorporating silver nanoparticles to form a coiled antenna. The system could pick up radio frequencies beyond the range of normal human hearing. In a similar manner, bioengineers might one day incorporate sensors into other tissues—for example, creating a bionic meniscus that can monitor strain.
Bioprinters are already demonstrating scientists’ remarkable mastery of biology and engineering. Back at Organovo, inside an otherwise unremarkable, neon-lit clean room, “Dallas” arranges human cells into intricate patterns that mirror those of nature. For young researchers like Vivien Gorgen, there’s little reason to stop and marvel at this. The machine has become just another tool—one that helps build tissue more precisely. A printer can put all the human pieces in the right places. But, as Forgacs continues to wonder, why do those pieces do what they do? Only life itself knows. At least, for now.
Steven Leckart is a writer-at-large for Pop-Up Magazine, which is created and performed for a live audience.
This article originally appeared in the August 2013 issue of Popular Science_. See more stories from the magazine here._