A 44-year-old British man was seemingly “cured” of HIV last week. Scientists working on the therapy say that the virus is now completely undetectable in his blood, leading to headlines announcing an “HIV breakthrough” that could “spell the end of the virus“.
But here’s the thing: It’s very difficult to determine whether HIV has been truly eliminated from the body, and even conventional antiretroviral therapy — which the patient was also taking — reduces HIV to undetectable levels. So pinning hopes on a single trial to prove a “cure” is a bit too premature, if optimistic.
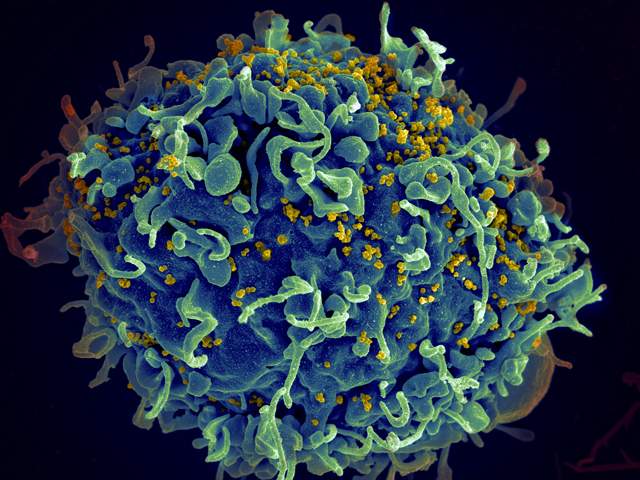
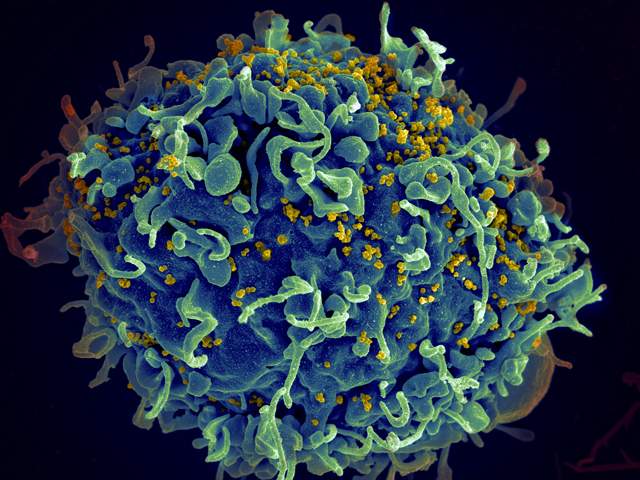
The hallmark of an HIV infection is that it targets very specific cells in a patient’s immune system, called CD4 T cells. These are white blood cells that usually detect intruders and corral a larger immune response to get rid of the invading bacteria or viruses. But HIV tricks these frontline soldiers and quickly inserts its own genetic material into the CD4 cells so that it can replicate inside them and use the cells to churn out more copies of virus.
Once infected, cells can’t get rid of HIV the way they can most other viruses. Taking combination antiretroviral therapy, however, stops HIV from reproducing and infecting new CD4 cells. Viral levels start declining and after two to three months of treatment, the levels of virus are so low that HIV is “undetectable” in a patient’s blood, says Janet Siliciano, an infectious disease researcher at Johns Hopkins University.
The problem is that most HIV tests measure the amount of viral RNA in free virus particles floating around in the blood and try to extrapolate the amount of virus hiding inside all infected cells. But in 1995, Siliciano’s lab found that some HIV remains invisible deep inside “resting” CD4 T cells. This silent reservoir can’t be measured by normal blood tests, she says. When people go off antiretroviral therapy, the virus rapidly resurges, and that’s when scientists realize that the virus was hidden somewhere inside the patient all along.
“Everyone has a different number of resting infected cells that are acting as a reservoir. They turn back on randomly, so it’s very hard to predict when someone will experience a viral rebound,” says Siliciano. That is why people with HIV must take antiretrovirals for the rest of their life, she explains.
The only way to know that HIV has left a person’s body is to test many different tissues — not just run a blood test — and keep repeating them over the years. Siliciano’s group is trying to develop one consolidated test.
Shock and Kill Strategy
One popular strategy in searching for a cure aims to obliterate the reservoir of remaining virus using a “shock and kill” approach. The idea behind it is that shocking the resting CD4 cells into waking up will force the virus inside them to become active as well. As HIV starts to rear its ugly head and put its mark on the surface of the infected cells, scientists can then boost a patient’s immune system to recognize and destroy HIV-carrying cells while they are vulnerable.
This is the technique used in the recent “breakthrough” by British researchers. The scientists, who hail from six different hospital centers in the UK, are testing an aggressive shock and kill regimen on 50 HIV patients over a period of about 9 months. The anonymous patient initially quoted in The Sunday Times is simply the first of the participants to have completed the treatment. Official results from the trial are not expected until 2018.
“I’m surprised that they would announce this in the press when they only have one patient and are not expecting all the results to come in until 2018,” says Stephen Morse, an epidemiologist and director of the Center for Public Health Preparedness at Columbia University. “There has been such a history of false optimism and false hope with HIV that you wonder why announcements like that are made.”
Even if the trial is a complete success, scientists will have to use caution in interpreting the results, according to Morse. Researchers will need to follow up on patients for several years, testing their viral levels regularly to make sure that HIV is truly eradicated from their system. They’ll also have to conduct a more extensive search for the virus to make sure it isn’t hiding in reservoir cells in the immune system or in other inaccessible parts of the body, such as cerebrospinal fluid or semen, Morse says. “We need a lot of good evidence before we can declare victory over HIV.”
To date, only one person has undergone that kind of rigorous testing. Timothy Ray Brown, who is also known as “the Berlin patient“, is the first and only person who can claim the distinction of being cured of HIV. In 2006, after living with the virus for 11 years and controlling his infection with antiretroviral drugs, Brown learned that he had developed an unrelated case of acute myeloid leukemia. He underwent chemotherapy and whole-body radiation that wiped out his immune system — and possibly the virus with it. Then he received a bone marrow transplant from a donor with a natural immunity to HIV. Researchers haven’t been able to find any trace of HIV in his blood or in multiple brain, gut, colon, and lymph-node biopsies since.
But bone marrow transplants have a high fatality rate, and there are just too many people with HIV — 33 million around the world — to make it a feasible therapy. And they may not even work consistently. Other patients who seemed to have been cured of the virus after receiving bone transplants still experienced a rebound of the virus after ditching their antiretroviral therapy — sometimes after nearly five years of being “HIV-free”.
Any new treatment that successfully eradicates the virus needs to be replicated in larger studies, says Siliciano. It also needs to match or surpass current standards of antiretroviral therapy, in terms of safety and accessibility of the drugs. Scientists also need to develop better, more sensitive assays to test for the presence of HIV. Only then will they be able to say accurately if a treatment is an effective cure for the viral infection.
“It’s a really hard, complex problem, and lots of scientists around the world are trying to work toward a cure,” she says. “But right now we have nothing that’s really close.”
