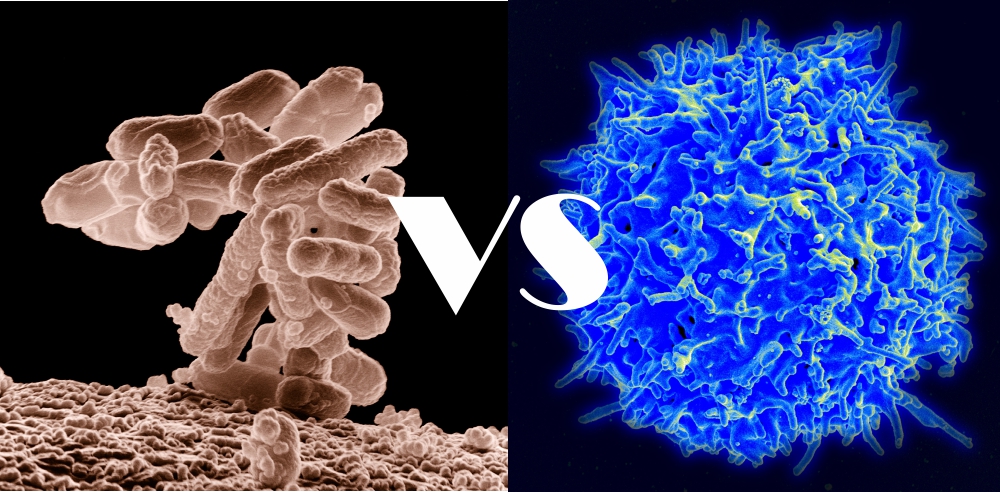
It’s become something of a catchphrase: bacteria outnumber us ten to one. That in itself is a bit of a misnomer as it’s only about three-to-one; your body has about 37 trillion cells while there are estimated to be about 100 trillion microbes. Even with the correction, we are without a doubt outnumbered by these invisible microorganisms.
Taking a look at the makeup of the microbial population, an even more fascinating revelation can be found. We all have a completely different census of species. Much like a fingerprint, no two people have the exact same types of microbes. The reasons for this difference have been examined and several factors have been unveiled including age, gender, diet, and lifestyle.
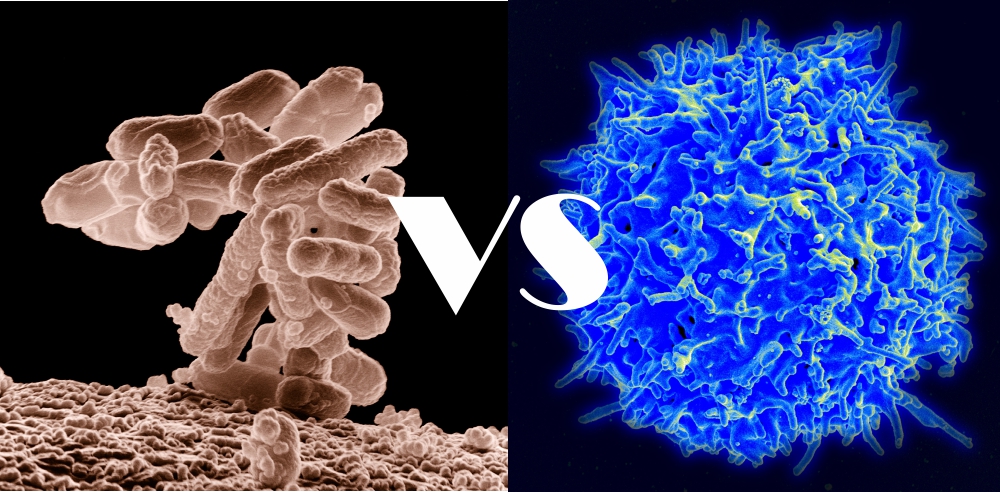
There’s also another player when it comes to our microbial uniqueness. It’s the immune system. Tasked with defending the human landscape, this collection of cells and molecules are constantly surveilling our bodies looking for any threats, whether chemical, biological, or microbial. Much like the microbes, each of us has a separate immune system and function.
But the immune system isn’t always about defense as it’s also involved in maintaining health. It’s involved in various other biological processes including wound healing, weight control, and mental health, to name a few. It most certainly would not be a stretch to propose immune function might be involved in determining what constitutes for us a healthy microbial population.
However, the evidence to suggest this has been less than convincing. Most of the time, studies have focused on how the microbes either cross-talk with the immune system or end up affecting immune activities by promoting traditional activities such as inflammation and autoimmunity.
Based on these studies and countless others, the picture suggests microbes may be in full control. We may be nothing more than serfs for a microbial liege. In essence, microbes are the masters and we are simply living and breathing to support them. If we and our immunities do not do as they command, we are sent into a variety of health consequences that reduce our quality of life and may inevitably kill us.
But this rather glum perspective may soon change thanks to the work of American researchers. Last week, they proffered a counterargument to the microbial master postulate. They found the microbes living in and on us may not be masters but instead migrants, given a pass to stay on our human grounds and co-exist with us.
The team worked with data already available from the Human Microbiome Project. They collected over fifteen hundred samples containing genetic information from 98 individuals. Using software, the mixed human and microbial genetic sequences were filtered and aligned such that they could identify what they called “human contamination reads.” These sequences, which came from humans and not microbes, were not useful at the time but for this study, they were genetic gold.
At the end of the work, sequences from 93 individuals were recovered and analyzed to determine any association with function. When this was complete, they had a collection of genes all linked in one way or another to the immune system. They were associated with a variety of functions from cytokine and chemokine response, to microbial recognition, and even fat regulation in the form of leptin signaling.
The next step was to determine whether there were any links between the immune factors and the nature of the microbiome. They found 83 such associations, far more than expected. As for which came first, the authors suggested this link had to be driven from the human as it was based in genetics. This meant the human condition laid the groundwork for the microbial migration.
An explanation and possible mechanism was presented using the link between the concentration of a probiotic bacterium, Bifidobacterium, and a host enzyme encoding for lactase. Although the immune system is not directly involved in milk digestion, it does play a role. For people carrying the enzyme, milk consumption is possible; for those that don’t, immunity may lead to symptoms of intolerance. Not surprisingly then, the bacteria, which do enjoy milk due to the lactose, end up in higher numbers in those expressing the enzyme.
Unfortunately, the authors didn’t go as far as saying we are indeed the masters of our microbial domain. Because this was an association rather than a “chicken-or-egg” study, they could not say whether microbial input over time contributed to changes in human genes. But they did suggest the results provide insight into the role of our immune system (at least genetically) in our microbial makeup and could motivate future research to answer the question once and for all.
The results also provide insight into how our own actions such as diet and lifestyle could contribute to health problems. For example, we can modify the microbial content through dietary changes, allowing even the most unwanted bacteria a chance to find a home. This in turn can work against the actions of the immune system and end up causing stress and chaos. If a poor diet is continuous, we could negate this genetic control and allow the microbes to dictate the conditions.
