You have to hand it to the immune system. The collection of specialized cells works endlessly throughout our lives to keep us safe. They are involved in almost every aspect of our daily life and are the front lines of defense against infection.
Normally, when a pathogen enters the body, an able immunity is capable of defeating most invasions. B-cells, T-cells, macrophages, neutrophils and others work in combination with one another to eliminate the threat and restore us back to health. It’s not always an easy process, however, and at times can lead to exhaustion. When this happens, our ability to fend off other invaders decreases. We essentially become more susceptible to other ailments.
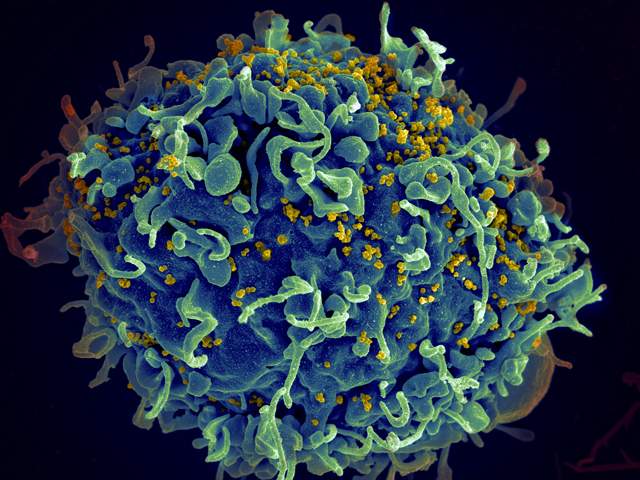
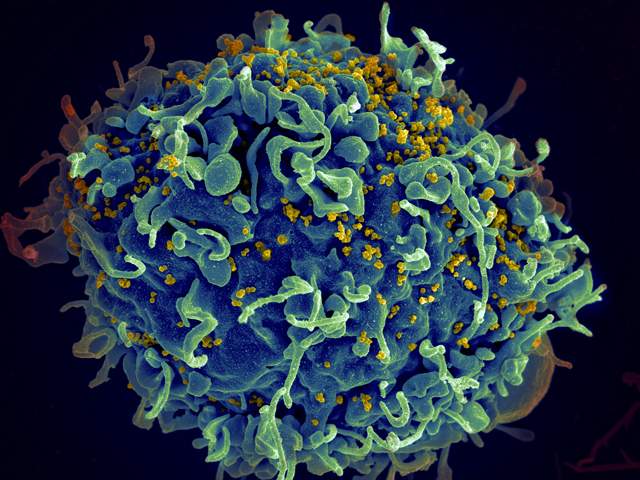
One of the most common causes of exhaustion happens with chronic viral infection, such as human immunodeficiency virus (HIV) or hepatitis C virus (HCV). Both of these pathogens have the ability to evade the defenses and maintain a presence for years. As this happens, the immune system continues to fight without any progress towards victory.
A vital immune cell in the fight against viral infection is called the CD8 T-cell. It has the task of finding these tiny pathogens and purging them from the body. The cell accomplishes this by either signaling an infected cell to kill the virus or, more viciously, to kill the infected cell altogether. Depending on the type of signal they receive their population can be controlled such that the response is just right for the situation. Once an infection is cleared, most of the cells die but some are kept around to serve as memory for any future viral attacks.
Unfortunately, when a chronic infection happens to occur, this process is interrupted and some of the CD8 T-cells lose their ability to function. This is known as exhaustion and can cause significant detriment against the current infection and worse, any new ones that happen to arrive. In HIV and HCV positive individuals, exhaustion is a serious concern as it may be the basis for even greater susceptibility to secondary infections.
The mechanism behind CD8 T-cell exhaustion hasn’t been fully understood but there has been some progress. Back in 2013, the condition was found to be reversible. On exhausted cells, a variety of proteins are expressed on the surface including one called the Programmed Death 1 (PD-1). This particular trigger is rather self-explanatory and has been called a hallmark of exhaustion. In HIV-infected individuals, this particular protein is also associated with progression of HIV infection. This could be reversed, however, with the induction of another cellular member of the immune system, the dendritic cell.
Although exhaustion theoretically could be reversed, there was still no clear mechanism. After all, PD-1 is only expressed in cells already programmed to die. Discovering the protein means the process has already reached a dire state. To get a better handle on the how exhaustion initiated and spread, they needed to find a more suitable biomarker candidate.
Last week, the answer may have been found. An international team of researchers discovered another marker associated with CD8 exhaustion. Perhaps even more importantly, this particular protein may also serve as a way to finally understanding how this condition occurs.
The group focused on patients with HIV or HCV infection with healthy individuals acting as a control. The team also looked at mice infected with the chronic infection, Lymphocytic Choriomeningitis Virus (LCMV). They collected blood samples and examined the blood for any sign of markers associated with exhaustion. They found one particular protein, called CD39, was higher on cells in chronically infected people and mice.
The choice of CD39 had to do with the function of the protein. It’s an enzyme that is normally found on a different type of cell, the regulatory T-cell, which is known to suppress the immune response. The cell uses the enzymatic action of CD39 as part of its suppressing activity. Finding this enzyme on CD8 T-cells in patients suggested an alteration of the usual immune response using one of two possible mechanisms. The first was causal in which these killer CD8 T-cells were forced by CD39 on other cells to shut down operations and eventually express the enzyme as a sign of conformity. The second, more likely scenario was correlation. In essence, CD39 was being expressed as a means of announcing the cell had giving up on the fight and was calling it quits.
The team tried to find some way to determine the actual reason using the mouse model. They took CD8 cells with a moderate percentage of CD39 positive cells and compared them to CD8 cells with a higher level of CD39 expression. As expected, the higher amount of the marker led to lower function. While this showed CD39 was correlated with exhaustion (in other words, a symptom), this could not prove whether CD39 was the cause of exhaustion. Other experiments would have to be performed to truly understand the early role of CD39.
Even though the overall relationship between CD39 and immune exhaustion wasn’t entirely figured out in this study, the group still found a good marker to identify the condition. Moreover, as CD39 was shown to be concentration-dependent on exhaustion, it may be able to identify troubles in the earlier stages and signal a possible downturn in health sooner. Though this may not offer a possible cure, for those who suffer with these chronic virus infections, this new discovery may help to foresee troubles ahead so lifestyle changes to improve health may be implemented.
