This afternoon, NASA astronaut Scott Kelly and Russian cosmonaut Mikhail Kornienko take off for a yearlong stay on the International Space Station. The record-breaking jaunt aims to help researchers understand how humans react and adapt to protracted stints in space. After all, we may soon find ourselves capable of traveling farther away from our home planet–and things can get weird while living long-term in zero gravity.
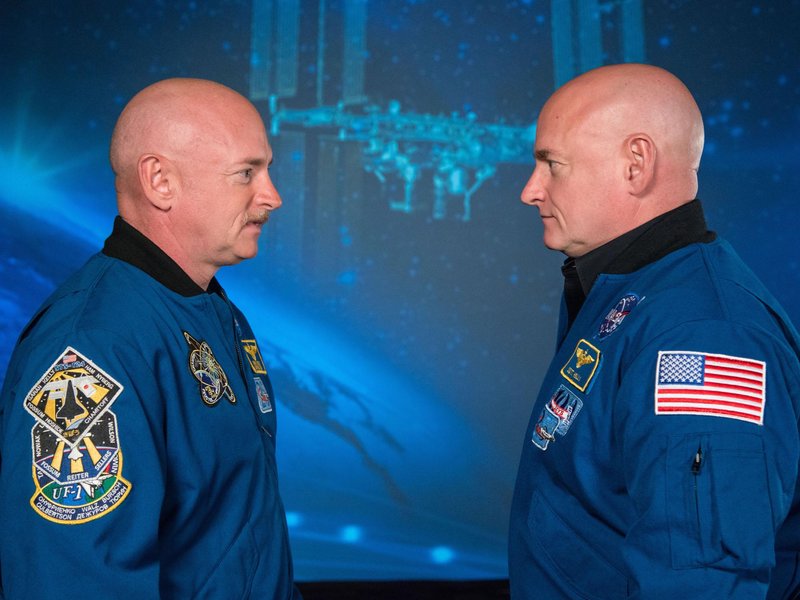
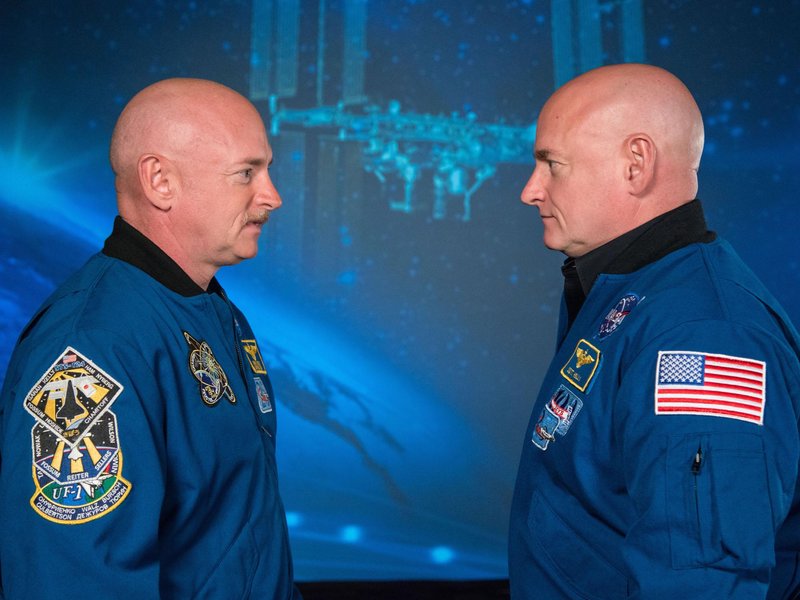
Fortunately, NASA’s study has the perfect control here on terra firma: Scott’s identical twin brother, retired astronaut Mark Kelly. In this unprecedented project, 10 investigations will collect and analyze genetic, molecular, and physiological data from both men. Scott and Mark will undergo the same tests at roughly the same time, providing researchers new clues about how spaceflight affects the body.
Among the many tests is one that’s been troubling scientists for some time: Why do more than half of U.S. astronauts experience changes in eyesight and intracranial pressure during long-term spaceflight? And could the results provide answers for how to treat eye disease on Earth?
In 2011, a survey of 300 astronauts found that nearly 30 percent on short-term missions and 60 percent on long-term missions suffered some loss of vision. Seven astronauts who were studied in-depth before and after a six-month run in space experienced a spectrum of changes: from fluffy off-white patches on the retina called cotton wool spots, to swelling in the “blind spot” of the eye and optic nerve, to a “flattening” of the eyeball shape.
Why do more than half of U.S. astronauts experience changes in eyesight during long-term spaceflight?
Researchers suspect that microgravity conditions cause body fluids such as blood to shift from the lower body to the head. This can trigger puffy faces and stuffy sinuses. “It feels like you have a really bad head cold,” says NASA scientist Jennifer Fogarty in a video about vision changes in space.
Testing this theory isn’t simple. Intracranial pressure is normally measured using a spinal tap—an invasive procedure in the best of conditions. Instead, scientists are using noninvasive methods such as MRI, ultrasound, and a light-based medical imaging technique called optical coherence tomography.
“Our goal is to understand and measure the fluid shift that occurs in space,” says UC-San Diego postdoctoral fellow Brandon Macias, a co-investigator on the project. “We hope to create a longitudinal map of changes: before, during, and after spaceflight.” What they find could have the potential to help treat common civilian eye issues, such as glaucoma.
Scott is trained to use an ocular ultrasound, which will observe blood flow, eye structure, and optic-nerve thickness. He will also employ a newer, safer technique for calculating intracranial pressure, using measurements made through the ear. A special device—called a chibis suit—puts negative pressure on the lower half of the body and will be monitored to determine if it helps move fluid away from the head.
Like any human study, there will be uncontrollable variables. For one, Scott has already spent quite a bit more time in space than his now-retired brother. Still, lead researcher Brinda Rana at University of California, San Diego, describes the study as “the ideal mouse experiment,” a nod to the popular use of genetically identical mice for scientific experimentation.
