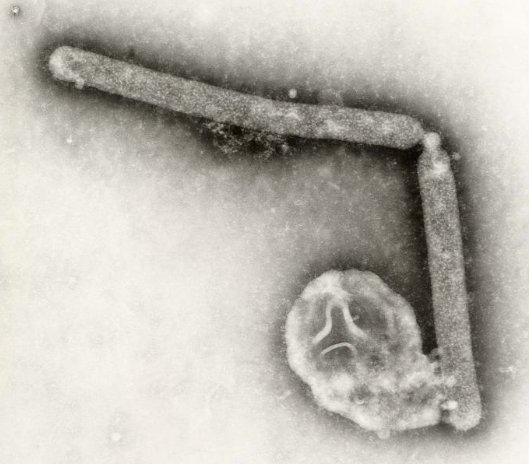
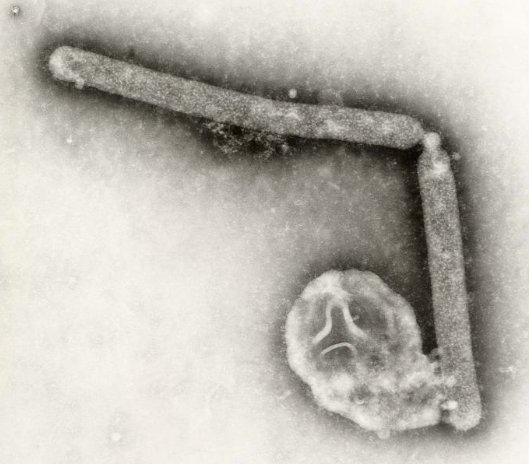
Only a few key mutations could cause the avian influenza virus to become airborne and transmissible among mammals, according to a controversial new paper publishing online today. In detailed research involving ferrets, researchers at the Erasmus Medical Centre in the Netherlands engineered a potent strain of the bird flu that could infect ferrets, and pass between them when the animals sneeze.
What’s more, this strain of engineered bird flu could mutate naturally, evolving the ability to attach to mammalian cells — potentially passing from human to human. Several natural strains of the avian influenza already have two of the mutations that are known to make the virus airborne, and they may only need two or three more to resemble the viruses engineered in two separate labs. Some scientists are hoping this research will give humans the upper hand in the fight against the flu.
Sander Herfst, Ron Fouchier and colleagues in the Netherlands set out to determine how much it would take for the H5N1 A flu virus to mutate into a form that can attack mammalian cells. They changed three amino acids to make the virus adapt to human cells, and they put this modified virus directly into the noses of ferrets, which are considered the best animal model of how humans respond to flu. The mutant virus did not transmit naturally, so the researchers designed an experiment to force it to adapt in the mammalian respiratory tract.
They did this by exposing two ferrets to two different flu variants, and swabbed their noses and throats every day for four days. The animals were euthanized on the fourth day, and their infected nasal tissue was used to expose another ferret. This process repeated six times, and then the researchers also induced the ferrets to sneeze. They collected the sneezes in a petri dish and then exposed additional ferrets to it. Viruses mutate quickly, so the team figured 10 generations was enough for it to adapt to replicate in mammals. It only took four.
Then the researchers determined what amino acid changes were present in these newly transmissible virus variants, and found that as little as five mutations were enough.
It may actually require a bit more than that, however, according to Vincent Racaniello, professor of microbiology and immunology at Columbia University in New York. “I wonder if in people, you might need different changes, or even more changes,” he said. “It’s important not to assume it is five.”
Months of controversy and a worldwide hiatus on flu research preceded the publication of today’s paper in Science, as well as a very similar paper in Nature last month. Now that the papers are in the medical literature, the reactions have been somewhat subdued. Some virologists say the fears were unwarranted — the research was careful and meticulous, and the recipe would be incredibly difficult to replicate — and others believe it would be worth a minimal risk, because understanding how flu mutates is crucial for preparation and vaccination efforts.
When he submitted his manuscript, Fouchier described his virus strain as “probably one of the most dangerous viruses you can make,” and other virologists and biosecurity experts balked. But Racaniello said the new paper is notably toned down from the original manuscript he read last fall. The paper and a related special section appear online today in Science Express.
“It’s not a biological weapon, that’s clear. It’s a nice piece of science,” Racaniello said, adding that it goes well with the earlier paper by Yoshihiro Kawaoka of the University of Wisconsin-Madison.
There’s a key difference between the two papers, and it has to do with just how the virus mutated. In Kawaoka’s paper, the virus was combined with DNA from a known human H1N1 strain, specifically the 2009 “swine flu” strain that sparked a pandemic. This is known as reassortment, and it’s one way that flu can mutate to “jump” from one species to another. In Fouchier’s paper, the virus was a H5N1 strain, with no human strains added. With some genetic modification on the front end, the virus was able to mutate sufficiently within one species to become airborne.
“He played God, if you will, with the genetics to get himself to a position where he didn’t have to reassort,” explained Jason Tetro, a microbiologist and coordinator of the Emerging Pathogens Research Centre at the University of Ottawa.
There’s another salient point common to both papers: The ferrets may have gotten the flu, but they didn’t die from it, at least not until their tracheas were directly injected with massive doses of the virus. The virus actually weakened as it took on mutations that made it airborne, said Dr. Earl Brown, a flu virologist and pathogen evolutionist at the EPRC. Captain Trips this is not.
“That’s got to make you calmer, if you are concerned about virulence,” Brown said. He and Tetro also added that the initial front-end changes both Kawaoka and Fouchier induced may not occur naturally.
Still, a statistical study that is published alongside Fouchier’s paper suggests at least some of them already exist. Given the large numbers of H5N1 reservoirs in nature and the virus’ proclivity for mutation, “it may simply be a matter of chance and time before a human- to-human transmissible A/H5N1 virus emerges,” the researchers say.
Dr. Derek Smith of the University of Cambridge said in a press conference that flu research is somewhat like trying to predict an earthquake or a tsunami. This study provides much more information to help assess risk, he said.
“We now know that we are living on a fault line,” he said. “What we have discovered … is it’s an active fault line. It really could do something. And now what we need to know is, how likely is that?”

