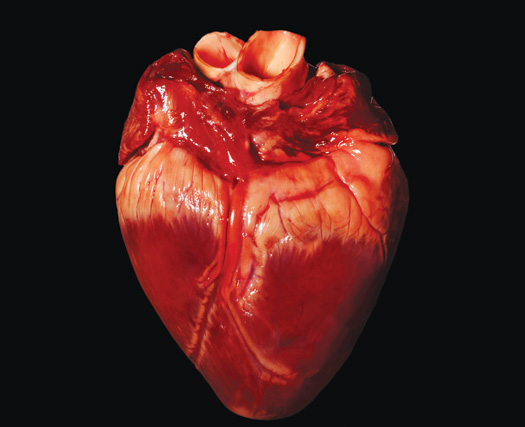
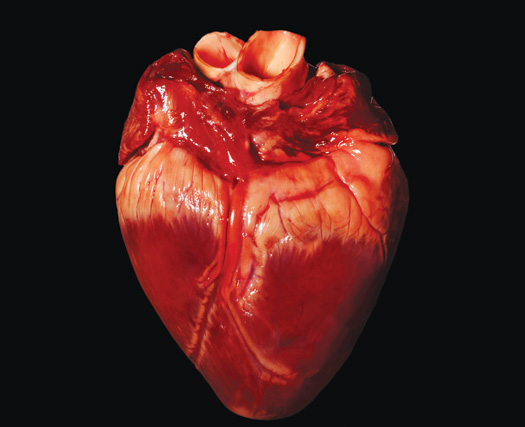
One of the most vexing problems that confronted surgeons after they completed the first successful human organ transplant, in 1954, was: Where would they get more organs? Medical researchers have since figured out how to transplant hearts, eyes and even entire faces. But half a century later, they still struggle to keep up with the demand for parts. For example, in the U.S., every year 1,400 people die awaiting livers and 4,500 more awaiting kidneys.
Part of the problem, of course, is that people want to hang on to the organs they have, both in life and death. But difficulties arise even with available organs. Because the human immune system is extraordinarily picky, the person at the top of the wait list may lose out to someone who’s a lower priority but a better immunological match. Transplant patients usually have to take debilitating immunosuppressant drugs. And even then, patients may reject the organ or die from opportunistic infections.
The body regularly probes proteins on cells’ surfaces to determine whether the cells belong or are foreign, and therefore dangerous. Three such proteins must match for blood donations. Doctors now pair organs with patients using a system that matches at least six protein variables, but even that isn’t enough to forgo immunosuppressant drugs. Now scientists are exploring several methods to trick the body’s immune system into accepting artificial and harvested donor organs.

Anthony Atala, a stem-cell specialist at Wake Forest University, conceived of a different approach than using organs from donors: making custom organs from scratch. In 1999 he first made a bladder for a patient from the patient’s own stem cells and is working to adapt the technique for kidneys and other organs. The method should be successful for people with nongenetic problems, such as spina bifida and smoking-related lung disease. For those with genetic illnesses, however, such as cystic fibrosis, muscular dystrophy and some cancers, organs made from their cells would most likely express the same problems that led the person to need a transplant in the first place. The solution? Work from someone else’s healthier stem cells, but match them to patients with extreme precision. Atala and his team have started collecting stem cells from amniotic fluid and placenta for a stem-cell bank that will contain more than 100,000 unique samples, sufficient for a close-to-exact match for 90 percent of Americans.
But the organs won’t be available for at least five years. And it will be a long time until such stem-cell banks are comprehensive enough to serve people with rarer DNA profiles. A simpler and perhaps more inclusive solution may be to coax bodies to accept a wider variety of organs (possibly including those from nonhuman animals). One possible method is to give patients an extra dose of mesenchymal stem cells (derived from adult bone marrow or umbilical-cord blood), which normally tame the immune system near where they reside. The treatment could help quiet immune reactions near the transplant site, leaving the rest of the immune system intact to fight infections. Researchers at the University of California at Davis are using the cells to help dogs tolerate canine-tocanine liver transplants. And over the past five years, others have used the treatment on dozens of human bone-marrow transplant recipients.
The solution? Work from someone else’s healthier stem cells.That approach is also not without shortcomings, though. Some researchers say that weakening the immune system, even in a discrete area of the body, could make patients more vulnerable to infections and that doctors should instead camouflage donated cells to sneak past the body’s defenses. The idea is almost as old as organ transplantation itself. For decades, scientists have struggled to hide foreign cells inside microscopic mesh capsules that would let the cells absorb nutrients and excrete waste molecules while hiding them from the immune system, which identifies cells by touch.
Viacyte, a company based in San Diego, is one of several research groups working to make containers that can house cells. It’s testing a bioartificial pancreas to treat diabetes: a plastic cartridge holding millions of cells that can release insulin in flux with the body’s need. The company says its prototype has successfully treated diabetes in hundreds of mice.
Scientists are studying all these possible solutions, but the treatments might not be available for some time. Meanwhile, there’s something everyone should consider to help get organs to those in need: signing up as a donor.
