On September 4, 2014, in Gothenburg, Sweden, his 36-year-old expectant mother lay on an operating table, suffering from preeclampsia—a pregnancy complication associated with high blood pressure. The baby’s heartbeat showed signs of stress. Normally the woman’s doctors might have taken a wait-and-see approach, treating her with medication and hoping to give the nearly 32-week-old fetus time to grow to full term of about 40 weeks. But this was no normal gestation. This was the world’s first human nurtured inside a transplanted uterus. He was the product of more than a decade of research. For years, no one had been sure he could exist in that womb—let alone be born. This was not a wait-and-see situation. As gynecologist and surgeon Liza Johannesson prepped to deliver the child via cesarean section, she was nervous. Not for the baby—she was used to delivering those—but for the uterus. It was 62 years old. A family friend of the patient, who had been born without her own womb, had donated it. The last time it had sustained a life was nearly three decades earlier. “We didn’t know what to expect,” Johannesson says. “We didn’t know if we were going to see [scar tissue] from the transplant surgery or how the new vessels would look, and how they would be positioned.” But as she cut into the woman’s abdomen, her scalpel revealed a uterus that, she says, “looked like it was 20. It reacted the same way it would if it were super young and super healthy. You couldn’t tell it was an old uterus.” The baby and the mother too both turned out healthy. It would be a month before the journal article announcing the birth would appear, allowing the Swedish-led medical team to tell the world: Uterus transplants are possible. And they can bear life.
That team has since delivered seven more babies via donated wombs, and this past November, with Johannesson’s help, Baylor University Medical Center in Dallas achieved the first such birth in the U.S. In February, a second. A leading organ-transplant center, Baylor has reported that two more women are trying to conceive as part of a large-scale clinical trial involving medical experts in nearly a dozen specialties. Under the guidance of transplant surgeon Giuliano Testa, Baylor hopes to build on Sweden’s research-based work to develop a proof-of-concept system that could be adapted around the world.
Hundreds of women’s fertility advocates have applauded Baylor’s work, and other transplant centers have contacted it to learn its methods. The need seems great.

Consider that kidneys, the nation’s most commonly transplanted body part, account for around 19,000 of the procedures each year. Then compare that to what may be as many as 2 million women in the U.S. with what doctors call “absolute uterine factor infertility.” Some have undergone hysterectomies due to cancer, fibroids, excessive bleeding, or uterine prolapse. Some are among the approximately 1 in 5,000 girls born each year without a uterus, a medical condition known as Mayer-Rokitansky- Küster-Hauser syndrome. And there is another category that hasn’t yet been tabulated—but almost certainly will be in the future: the hundreds of thousands of women who represent a portion of America’s 1.4 million transgender people. They too might one day be able to choose to bear children thanks to this new surgery.
Of course, there are caveats that need to be negotiated before the uterine transplant can become an everyday surgery. First, there are ethical concerns. Critics question the necessity of the procedure, given that women have other paths to motherhood, such as surrogacy and adoption. Some wonder if surgeons are undertaking the challenge simply because they can. And then there are the risks. The donor must undergo a medically unnecessary surgery to remove her womb. The recipient must undergo three: one to insert the uterus, another to deliver the baby via C-section, and a third to remove the organ after birth. (Doctors do not want patients to spend a lifetime taking immunosuppressive drugs, which come with risks, to prevent rejection of a part not needed for survival.) Finally, there are the costs, which Testa estimates at around $250,000, putting the operations beyond the reach of any but the most affluent, and perhaps the most desperate.
Undeniably, the research that went into the procedure is groundbreaking. And Testa thinks Baylor’s clinical trial—monitored and supervised by the hospital’s internal review board and following the rules of the United Network for Organ Sharing, a nonprofit that manages the nation’s organ transplant system—will one day allow thousands of women to carry children. “It makes no sense to innovate if it stays for only one case,” says Testa. “It becomes a stunt. We’re talking about helping people at large. I hope this is the spark that turns into a furnace.”
In 1931, a German surgeon performed the first-known uterine transplant, on a Danish transsexual named Lili Elbe. She died soon afterward, probably due to tissue rejection. Decades later, in 2000, a Saudi Arabian woman who had lost her uterus during childbirth wanted another baby and came up with the transplant idea on her own. Her doctors agreed to attempt the procedure; the implanted womb lasted three months before its tissue began to die and it had to be removed. The woman survived. “They were criticized,” says Johannesson, because of a lack of clinical and ethical transparency and the procedure’s failure.
But other, more-rigorous attempts were underway at that time, none more advanced than that of Swedish transplant surgeon Mats Brännström, who had faced a similar patient request in 1998. Rather than plow ahead in the dark, he created a team at the University of Gothenburg and attempted to puzzle out just how to do the surgery in a way that wouldn’t fail. Johannesson joined his team in 2008 during her gynecology residency, having decided to pursue her doctorate in this area.

The first goal of the study was to perfect the surgery in animals. The team had started with mice and rats, removing and attaching uteruses under a microscope. Later, Johannesson headed up the final phase of research: working on nonhuman primates, specifically baboons, whose abdomen reflects the anatomy she would face in people. For the next several years, she traveled to Nairobi, Kenya, eventually performing uterine transplants on 66 such human-resembling primates.
The goal in all these animal surgeries was twofold. Connect the uterus to the body and secure its blood flow. To attach this triangle of tissue, Johannesson learned to stitch it to the vagina and a group of ligaments. The uterus, which in humans weighs 2 ounces and is about the size and shape of an upside-down pear, has multiple blood supplies (two arteries and two veins) that keep it, and a fetus, alive with oxygen and nutrients. During a pregnancy, blood volume increases by up to 50 percent, enlarging these passages. (Both the Swedish and Baylor teams require that a donor has already borne a child, as proof that the organ works.)
During the animal trials, Johannesson monitored each patient for rejection. Not all transplanted organs react the same way in a host body. There are a slew of soldiers in our immune system whose job it is to detect foreign objects and eliminate them. Watching how rejection works on these foreign body parts helped Johannesson and her team stave it off with the right cocktail of immunosuppressive drugs.
By late 2011, they were confident they could succeed in humans. But it would take the Swedes four months to convince a national medical ethics board that the surgery could be morally justified. The group wrestled with dozens of questions: How do you explain the risks and benefits? Is it right to offer hope when results aren’t guaranteed? Why perform such a procedure when so many children need adopting? Why perform it when surrogacy is an option? That option, Johannesson points out, is similarly morally fraught, since it requires women to pass the risk of pregnancy to another person. In the U.S., it’s often handled through a paid business deal, but in some states and countries, including Sweden and much of Europe, surrogacy is illegal.
“It’s a necessary thing to do,” Johannesson says of the ethics discussions. “These are people’s lives we have in our hands. We need to be sure we’re [making] good decisions. We have to question ourselves.”
By spring 2012, the research group had received permission to move forward. Two years later, the first patient gave birth to a boy. A year after that, Johannesson joined Testa in Dallas as he prepared a trial that, if successful, would allow them and others to scale up the procedure to help thousands of women.
To ensure the success of their trial, and their patients’ health, the Baylor team requires subjects to meet strict criteria. Recipients must be extremely healthy and no older than 35, to reduce the chance of pregnancy complications. Both the donor and the intended mom must undergo psychological evaluations to determine their reasons for participating and to confirm that they can provide informed consent.

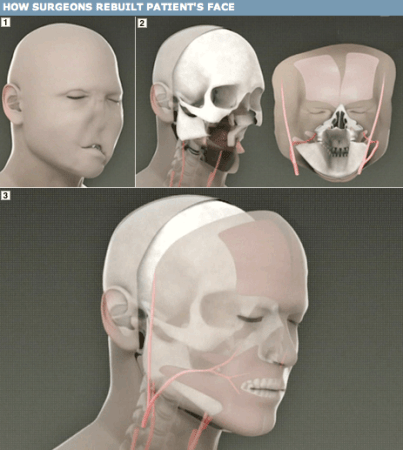
When it comes time for surgery, the donor and recipient are prepped in adjacent operating rooms. First, a gynecological oncologist removes the donor’s uterus through her abdomen. Normally, in a hysterectomy, the surgeon begins by cutting the blood supply to the organ. But because in this case he must maintain that supply to keep oxygen and nutrients flowing to the organ, he does this last. “This means there is much higher risk of accidentally nicking an artery and having to deal with blood loss,” says team surgeon E. Colin Koon, who is an expert in radical hysterectomies.
Koon must remove more tissue than he normally would; he takes more of the blood vessels than in a typical hysterectomy. “It’s a very big dissection,” he says. Also the head of Baylor’s robotic surgery, Koon is exploring the possibility of performing this procedure less invasively, extracting the organ through the vagina rather than the abdomen. This would be less traumatic for the donor, who must currently stay in the hospital for up to six days after the surgery so staff can monitor her recovery.
Minutes after removal, a team member takes the uterus into the other operating room. There, the surgical plan follows a 3D map of the inside of the recipient’s abdomen. This has been created by the team’s radiologist and imaging specialist, using a combination of ultrasound, MRI, and CT angiography. A dye added to the blood “lights up” the arteries and veins, some no more than a millimeter in diameter, says team radiologist Greg de Prisco. Because blood vessels aren’t always in the same exact location in every body, the dye lets doctors pinpoint their target. “The surgeon wants to know before they go in: ‘Where should I cut?’” says de Prisco.
Testa and Johannesson then get to work. They insert the uterus and attach it to the blood supply, suturing the organ’s arteries to an aortic vessel that runs down into the leg. After that, they attach the vagina and anchoring ligaments, and the transplant is complete.
Three to six months later, provided the patient has experienced consistent menstruation, IVF doctors implant an embryo, the result of eggs harvested earlier from the mother and sperm from her partner. She will be able to feel the baby move, but, because surgeons do not connect the mother’s nerves to the baby’s cocoon (it is a complicated and medically unnecessary step), she does not experience labor pains. A lack of working nerves also makes doctors unsure if the uterus will contract normally, so they deliver the child via C-section. Vaginal birth might be possible in the future, Johannesson says, though it is not a part of the current trial.
It’s early February, and Kristin Wallis is on the phone with a woman interested in receiving a uterus. Wallis is the nurse coordinator for Baylor’s clinical trial team. She vets prospective patients and women wanting to donate. Since Baylor announced its trial in 2016, more than 500 women have emailed or called Wallis. She is an advocate for each patient in the trial, following them through every stage of surgery, sometimes sleeping in the hospital with them, and answering their calls day and night.
Baylor has not yet announced a second trial, and its current one has already selected all of its recipients. But Wallis still listens to everyone’s tale in case they could be candidates for future studies, and also because she feels each woman deserves to be heard. Today’s caller tells Wallis she lost her uterus to fibroids when she was young. Unfortunately, Wallis quickly knows the woman is ineligible. She’s too old and has a heart condition. Still, Wallis spends 45 minutes sympathizing with her, while also telling her candidly that she cannot have a transplant.
“If I cut them off after the first sentence, they don’t get to tell their story,” says Wallis, after she hangs up the phone. “I do want to hear them, but it does take a long time.”
Increasingly, callers might have elsewhere to turn. According to the U.S. National Library of Medicine, doctors have either started or plan to start as many as 12 additional uterine-transplant trials around the world. This past March, in an attempt to spread its knowledge, Baylor hosted dozens of surgeons from across the country (from places such as Harvard, the University of Pennsylvania, and the Mayo Clinic) eager to learn about setting up their own programs.
That widespread adoption offers hope to the transgender community, which has been watching the progress of uterine transplants. Katelyn Burns, a member of that community and a freelance journalist who covers its issues for media outlets such as The Washington Post and Vice, says circles of trans women regularly discuss one day giving birth. Many, says Burns, would opt for the surgery if it were made available. “There’s a quiet confidence” that they will gain access to this, says Burns, adding, “If I were young enough, and if I could afford it, I would probably try for it.”
Right now, uterine transplants are experimental. That means risks abound for everyone involved. Even if patients who receive the organs remain healthy, there’s always a chance they could undergo a painful operation only to have it fail. But even recipients whose new wombs have been unsuccessful have expressed to Testa and Johannesson they were glad to have gone through the process. They contributed to furthering the science. Their uterus’s failure, though it did not give them children, still moved the world that much closer to fulfilling for their fellow women what once had been an impossible dream.
Johannesson doesn’t mind when people criticize (it’s a part of the process) and ask if it’s really worth it for anyone to undergo experimental surgery to bear a child. After all, surgeons have been successfully grafting penis replacements on men since 2014. Is a uterus really less essential? Zachary Rubeo, the team’s maternal fetal medicine specialist who monitors the transplant pregnancies, notes that since medical science has tackled many other aspects of infertility—from hormone injections and freezing eggs to artificial insemination and IVF—stopping at women who don’t have a functioning body part is discriminatory. “To look them in the face and say, ‘We won’t help you,’ that’s sort of unfair,” he says. Medical science has made pregnancy unnatural for decades. But there’s nothing more natural than giving a woman the chance to give birth to her own child.
Erin Biba is a freelance journalist based in New York City. She writes about science for publications such as the BBC and Scientific American.
This article was originally published in the Summer 2018 Life/Death issue of Popular Science.