

Hannah Hoag is a Toronto-based science journalist and editor whose articles have appeared in Nature, Science, Biographic, Wired, and The New York Times, among other publications. She is allergic to wasps, hornets, and yellow jackets, and is currently undergoing venom immunotherapy treatment. This story originally featured on Undark.
One morning in the fall of 2019, Zach Techner stepped into a heavily woven white beekeeper’s suit, pulled on rubber boots and thick orange gloves, and wrapped duct tape around his cuffs and along the zipper. He slid safety glasses over his eyes and a netted hood over his head and zipped it shut. He was preparing to collect one of the most dangerous wild creatures in the United States: yellow jackets.
Techner carried a portable vacuum he had MacGyvered into a wasp-sucking machine to a low thicket of blackberry brambles. A dozen of the flying insects made large descending loops towards their nest in the ground. Over the next 45 minutes, he siphoned the yellow jackets—uninjured but surely a little upset—into a plastic juice jug. He stored the trapped insects beneath a layer of dry ice in a cooler to kill them quickly—and avoid damaging the proteins in their venom.
Wasp collecting isn’t always so uneventful, Techner warned. Yellow jackets can attack—especially in the fall when colonies swell and food is scarce—with sharp stings or by contracting their abdomens to spray their venom in their assailant’s eyes. “When you’re in the middle of a nest and there are thousands of them attacking you, hitting the veil, the venom can still get into your eyes,” he says. “It hurts really bad. It can be blinding.”
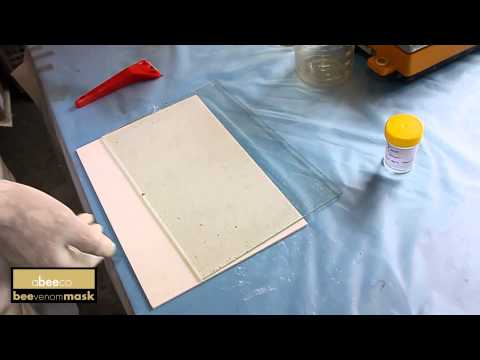
Techner owns Cascadia Venom Collection, based in Rochester, Washington. Like dozens of other professional collectors across the country, he is paid by the pound to collect yellow jackets, wasps, and hornets, and ship them to medical manufacturing companies in the US and Europe, where the venom is transformed into lifesaving medicine for those who have severe allergic reactions to stings. (Honeybee venom collection is a little different; due to their ecological importance as pollinators, beekeepers harvest the venom by inducing live bees to sting glass collection plates.) Each year, tens of thousands of people in the U.S. with venom allergies are deliberately injected with small doses of venom over three to five years to desensitize their immune systems to the allergen and, hopefully, eliminate their risk of anaphylaxis, a potentially lethal allergic reaction.
In a good season, Techner and his team will bag more than 400 pounds of stinging insects. European paper wasps, which nest together in small numbers, garner the highest price at about $2,000 per pound. Yellow hornets and yellow jackets, which have larger nests that can reach thousands of individual insects, might bring in closer to $600 per pound.
Yet despite a seemingly endless supply of stinging insects, the venom supply chain has been showing signs of strain. In countries and regions with a single supplier of venom extracts, including Canada, Australia, Southeast Asia, and South Africa, there has been, on occasion, a total lack of product available for patients to start or continue venom immunotherapy. And now due to recent changes in venom manufacturing, the US could be equally vulnerable.
In a 2016 letter, the Food and Drug Administration cited problems with procedures put in place to prevent microbial contamination at a Denmark-based manufacturing facility owned by ALK-Abelló, which held about two thirds of the North American market for venom products at the time. Later that year, the company told those customers it was no longer able to fill orders for six venom extracts—honeybee, wasp, white-faced hornet, yellow hornet, yellow jacket, and a cocktail from several wasp species.
In early 2018, ALK announced it would eliminate the North American product line entirely. The line was not a high-profit one to begin with, and the upgrades its production facilities needed for FDA approval were too expensive, says Jeppe Ilkjaer, a company spokesperson. The three products ALK makes for Europe, on the other hand, experienced some disruptions but are back on the market today.
For several months, the only remaining North American manufacturer, HollisterStier Allergy, a division of Jubilant Pharma that is based in Spokane, Washington, struggled to meet the demand of the US and Canadian markets. Wasp collectors had freezers full of ready-to-ship insects, but allergists in the US and Canada scrambled to get their hands on venom extracts to treat their patients. They stocked up on the extracts they could find, rationed doses, borrowed from friends, tried to switch suppliers, and stretched the time between injections. Eventually, HollisterStier bumped up its output to fill the void in North America, and the FDA approved a second production line around the beginning of this year.
Aside from the microbial and mechanical problems that could shake up production, another risk, allergists say, is that HollisterStier could leave the business altogether. The US market for venom immunotherapy is small (about $20 million per year) compared to other allergy drugs, such as nasal sprays, which exceeds $2 billion annually. Yet Chris Preti, president of HollisterStier Allergy, says the company is committed to producing venom extracts. It has shored up its supply of raw material by entering into agreements to buy wasps, hornets, and yellow jackets from their collectors for years out, and the company has invested in a third production line that should be running by 2024. “If we left there would be tens of thousands of patients that we service with no option,” he says.
Still, the North American market now relies on a single company for venom extracts, unlike European countries, which have a range of suppliers. HollisterStier temporarily ran into production troubles that interrupted the supply of several of its venom extracts, causing additional shortages this year in Canada, although not in the US. But the potential for a problem is there, says David Golden, an allergy expert and associate professor of medicine at Johns Hopkins University: “One day there is going to be no venom in the US.”
The sting of a yellow jacket, hornet, or wasp is sharp, searing, and hot. For most people, it causes redness, swelling, itching, and some pain, but is relatively uneventful. Yet for those allergic to insect venom, the first sting triggers an exaggerated and misplaced immune response that sets off a chain of events and can lead to a life-threatening anaphylactic reaction should they be stung again.
A single insect sting delivers a dose of venom so tiny that it would seem insignificant. Yet the complex mixture of allergens, toxins, and proteins can destroy cells, spread pain, overstimulate nerves, and drive down blood pressure for those who are allergic. The skin itches, hives erupt across the entire body, and the throat may begin to close. Dizziness and loss of consciousness can occur, along with stomach cramps, vomiting, and diarrhea. The body can collapse in as little as 10 minutes.
The rates of insect venom allergies typically fall into a range of 5 percent to 7.5 percent of the general population. One .S study found sting injuries from bees, wasp, hornets, and yellow jackets led to an estimated 200,000 trips to the emergency room annually between 2001 and 2010, and another found a 59 percent increase in ER visits for venom anaphylaxis between 2005 and 2014. A European study of severe allergic reactions found that one fifth of anaphylaxis cases among children and nearly half of those documented in adults were due to insect stings.
Even though insect stings are not usually fatal, they kill more people in the U.S. each year than any other wild animal, including bears and snakes. Data from the Centers for Disease Control and Prevention show 1,109 deaths due to hornet, wasp, or bee stings occurred between 2000 and 2017, an average of 62 deaths per year. Globally, these numbers are widely thought to be underreported, as allergic reactions to stings are sometimes mistaken for heart attacks or sunstroke. Allergists say there is far less public awareness about the risks that come from insect stings than from other allergens like peanuts.
Venom allergies have plagued humans for thousands of years. At the end of the 12th century, the philosopher and physician Maimonides offered tips on dealing with stings and bites of venomous animals, including bees and wasps, in his “Treatise on Poisons and Their Antidotes.” In another “Treatise on Poisons” first published in 1814, French toxicologist and chemist Mathieu Orfila gave an early account of death by wasp: In 1776, a gardener in Nancy bit into an apple in which a wasp was lodged and the sting “killed the poor unfortunate man within a few hours.” But it would take nearly a century more before physiologists Charles Richet and Paul Portier would describe anaphylaxis in their Paris laboratory.
Beginning in the 1930s, wasp and bee allergies were treated by injections of extracts from whole ground insects to desensitize the immune system. In the late 1940s, Mary Hewitt Loveless, an immunologist at Cornell University Medical College, challenged this approach, arguing that the allergens were concentrated in the venom. In 1956, Loveless ran a small uncontrolled study that showed that injecting progressively increasing doses of venom in her patients could eliminate future anaphylactic reactions. For years, she and her trainees would collect the insects with butterfly nets or nab entire hives and remove their venom sacs by hand. Loveless’ research, however, was largely ignored for two decades.
It wasn’t until 1979, following the results of a placebo-controlled study conducted on 59 soldiers, that the FDA approved venom immunotherapy. Venoms were the first standardized allergens to be used in medicine, and are considered to be as much as 98 percent effective—depending on the species—at eliminating venom allergies.
At Hollisterstier’s manufacturing facility in Spokane, Washington, Pete Colomb, the associate director of manufacturing, strode through a maze of corridors in a white lab coat and blue hair net. In addition to making venom extracts, the company produces dozens of other allergens. In one storage room, glass jars full of pollens—red alder, mountain cedar, bottlebrush—dust mites, cockroach, cattle hair, aspergillus, and other allergens lined the shelves.
Outside the dissecting room, Colomb stepped into disposable booties and onto a tacky mat to avoid tracking in any dirt or debris. Three women—hair pulled back and fingers enclosed in black disposable gloves—sat behind piles of dead yellow jackets. One of the dissectors gently rolled an insect between her fingers to warm it and then bent it to separate the stinger from the body. She plucked the exposed venom sac, no bigger than a tomato seed, from the insect with a pair of sharp pointed tweezers and slid it into a plastic tube of cold preservative.
It takes these dissectors up to 520 hours of work and 130,000 insects to produce a batch of venom extract. The process has been slowed somewhat by restrictions put in place during the COVID-19 pandemic.
Many of those who are allergic to stinging insects aren’t even aware a treatment exists. After a sting in 1994 sent Julia Magnusson to the ER, dizzy and covered in hives, she assumed she had a bee allergy and tried to avoid them. It wasn’t until December 2018, more than 20 years after her initial sting, that her son’s allergist told her she could be tested and treated with venom immunotherapy. “Sixty percent of individuals who have fatal reactions have been diagnosed, but not treated,” says Vera Mahler, a dermatologist who also studies allergies at the Paul Ehrlich Institute in Langen, Germany, the federal research institute that assesses and regulates vaccines and biomedicines in the country.
It turned out Magnusson was allergic to yellow jackets, yellow hornets, and white-faced hornets, not bees, yet she still stalled her treatment for months, worrying about a bad reaction or anaphylaxis. But she had kids and spent a lot of time running and biking in the woods. During the first injections, her arm “would be swollen from shoulder to wrist, like a big fat elephant arm,” she says. Her reaction to the allergy shots eventually subsided, and she now has the confidence that if she’s stung again, she can “get out of the woods alive.”
Drug shortages have become persistent global problems over the past several decades. In 2018, the FDA reported a scarcity of more than 50 drugs and biologics, largely sterile injectable medications used for chemotherapy drugs and anesthetics. In the U.S. most shortages for biologics—such as vaccines or venom extracts—are related to quality problems at the manufacturing facility.
When there is an alternate drug available, patients are less likely to suffer. Germany, for example, saw no disruption during ALK’s manufacturing issues because the country has several other products from companies in the Netherlands and the U.K. approved for sale. Australia, which anticipates a non-critical shortage of several venom extracts until April 2021, has a provision in place that provides the temporary approval of select unregistered products to cover the gap.
Some allergists would like to see the North American market opened up to European products to avoid future shortages. Part of the barrier lies in the way the products are approved. The FDA has a US reference standard for potency, which it distributes to manufacturers, whereas in Europe, products are compared to the company’s own in-house standard. As it stands, a product in use in Europe wouldn’t automatically be approved for use in the US—a European company interested in entering the US market would have to create a new product that adheres to the FDA standard. “There is no compromise between the two approaches,” says Stefan Vieths, who studies the molecular basis of allergies at the Paul Ehrlich Institute in Germany. “If you agree to one, it would mean a lot of work to try to meet the other.”
In addition, the FDA would likely require “multimillion-dollar clinical trials involving sting challenges,” says Golden, referring to the act of intentionally stinging people by holding a yellow jacket, for example, on the arm of a volunteer until it stings them, which comes with the risk of anaphylaxis. “So, we’re stuck,” he says.
“Some people think the FDA should relax their standards and accept some of the research that has been done in Europe, accept the results of the studies,” says J. Allen Meadows, an allergist in Montgomery, Alabama, and the outgoing president of the American College of Allergy, Asthma, and Immunology.
In a commentary published in the college’s medical journal in 2019, Meadows and his colleagues suggested specialists might target a federal program that provides incentives for companies to develop products called orphan drugs for rare diseases that usually affect less than 200,000 people in the US. Since the program was started in 1983, it has helped bring more than 600 drugs and products to market, including five snake, scorpion, and spider antivenoms.
Even so, the gap between the cost of treatment and the amount that allergists are reimbursed by insurance carriers and Medicare has forced some small practices to stop offering venom immunotherapy. “Immunotherapy is a substantial piece of our revenue, but venom is, month-to-month, the only therapeutic element that is consistently in the red,” says James Tracy, an allergist and immunologist in Omaha, Nebraska, who is a managing partner at what he says is a multi-million-dollar practice. “The harsh reality is that there are many practices that can’t afford it.”
Despite the shortage of doctors who are willing to take the financial hit, “in the short-term, we’re probably OK,” Tracy says. “But if there is another supply issue—it happened to ALK—if you had a double whammy, it would be a problem.”
