This month, the FDA approved a new drug called Inflectra, which could be used to treat a handful of inflammatory conditions such as Crohn’s disease, psoriasis, and arthritis. That in itself might not be so surprising—the FDA approves new drugs all the time. But this is only the second biosimilar drug to go on the market in history.
What does that mean?
The first thing to understand is the difference between small-molecule drugs and biologics. Most drugs fall into these two categories, though the distinction is probably most important to the companies making the drugs, to doctors considering their side effects, and to pharmacists, who have to store some of them under special conditions.
So what’s the difference?
Small-molecule drugs are, as you might expect, small and fairly simple in their structure. They are synthesized from chemicals in a consistent process so that manufacturers can be sure that each pill has the same effect every time. Drugs like aspirin (acetaminophen) and common allergy medications (Acrivastine) are small-molecule drugs.
And what’s a biologic?
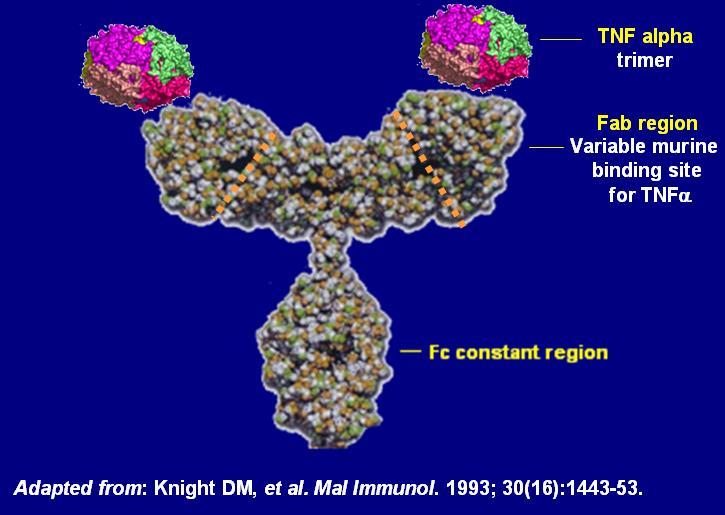
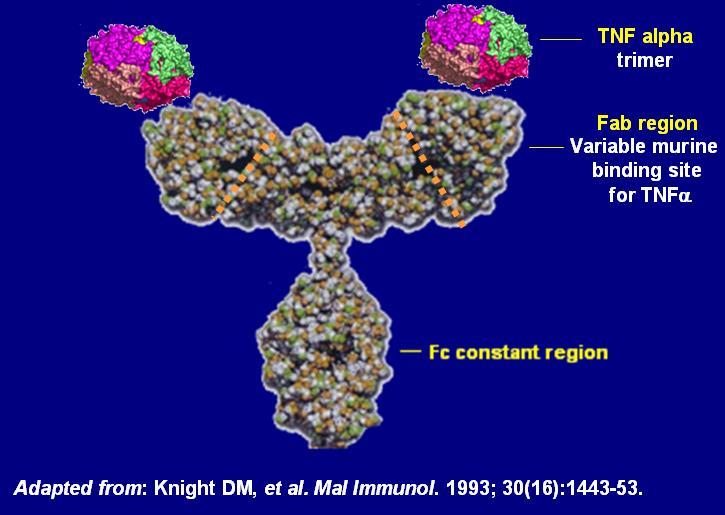
Biologic drugs are made by a living cell, typically an engineered bacterium or a yeast. That gives them the capacity to be chemically much more complicated—if small-molecule drugs are a tricycle, biologics are a space ship, one expert told Fortune. They’re bigger and heavier, and often less stable, so they require special handling like refrigeration.
For biologic drugs, compounds are collected from living systems. Sometimes those are animals such as cows, mice, rabbits, goats, and even humans, says Mary Wahl, a recent fellow in molecular biology at Harvard who now works at Microsoft. Other types of drugs are extracted from plants such as tobacco and microorganisms, those that occur naturally as well as those engineered by scientists.
And that means there’s no way to guarantee that each dose of the drug will be identical.
Biologic drugs can help with lots of different conditions in the body, like monoclonal antibodies to fight cancer, or Neupogen to boost white blood cells for patients undergoing chemotherapy.
Great. So a biosimilar is what?
When the patent surrounding a biologic’s formula is no longer protected, multiple companies can release a drug with the same chemical recipe, driving the cost down. That new biologic drug is a biosimilar.
That’s important because biologics are blockbusters—in 2014, six of the top 10 best selling drugs in the world were biologics, according to the New York Times—and those patents have started to expire in the past few years, say Wahl. “[Those expired patents] open the road for other companies to start developing biosimilars,” she says. It’s understandable why there’s been a bit of a delay before biosimilars have hit the market, since biologics have to go through more tests because of how they are synthesized.
Biosimilar, not bioidentical?
“Molecular structures of small-molecule drugs are specified exactly. Even a small change… could radically alter their function in the body,” Wahl says. Since biologics are created by living (error-prone) cells and are significantly more complex, generic versions are merely “similar” to the original drug–they might have slight variations in their structure and require more evaluation to make sure those variations won’t change how the drug works in the body. “If we can’t specify the shape of the original drug, we can’t specify the shape of generic versions, either,” Wahl adds.
Are biosimilars good or bad new for patients?
The upside of biosimilars is that consumers can get biologics for cheaper. By some estimates, that could save the U.S. $250 billion over the next decade. That’s good for everyone, provided that biosimilars work as well as the more expensive ones.
But there’s a downside, Wahl says. Drug companies are investing in biologics and biosimilars because they think they can keep their patents for longer. Since biologics are made from living cells, it takes more work for drug companies to prove to the FDA these drugs are safe and effective. “Drug companies might invest in (new) biologics because they perceive that biosimilars will not be developed even after the patent expires, because competitors would have to make a relatively large investment to develop a biosimilar and get it approved by the FDA,” Wahl says. And while biologics seem to treat some conditions, such as cancer and autoimmune disorders, better than small molecules can, Wahl isn’t convinced that biologics provide a clear advantage overall.
“Drug companies have a strong incentive to create the perception that biologics are more effective.”
“Biologics are often more expensive than small-molecule drugs, and because of the difficulty in bringing biosimilars to market, they may also have higher profit margins: this is why drug companies have a strong incentive to create the perception [among doctors] that biologics are more effective than small-molecule alternatives.” she says. “Intellectual property would last longer and their profits would be higher. But I’m not convinced that small molecules couldn’t accomplish the same thing.”
Small molecules mostly cause fewer side effects, and are unlikely to cause life-threatening conditions such as a cytokine storm. And if pharma companies are investing all their resources into biologics and biosimilars, they might be ignoring the potential of small-molecule drugs that can do the same thing and ultimately be better for the patient.
Inflectra, approved by the FDA earlier this month, is chemically similar to Remicade, the biologic that treats many of the same inflammatory diseases. The first one, called Zarzio, was approved in 2015 and helps chemo patients make more white blood cells (the “generic” version of Neupogen). These are the first of what will likely be many more biosimilars that will hit the market in the next few years.
