Those are the now oft-quoted words of Anne Schuchat, the principal deputy director of the Centers for Disease Control and Prevention describing the Zika virus situation. Since the announcement of the arrival of the pathogen in Brazil late last year, the news seems to be getting worse, not better. With each week it seems, we are learning about a new region becoming affected or of another side effect from infection. All the while, concerned Americans are calling for researchers to find answers.
Unfortunately, the calls have not been answered as a $1.9 billion request for Zika funding has stalled in Congress. In its place, some $589 million will be allotted. This means priorities need to be determined to gain the most from less. However, this is not easy as two diametrically opposed options emerge, both of which have utmost importance to Americans.
The first is to better understand the mechanisms behind various symptoms and conditions associated with infection. Microcephaly was the first to be documented but we now know of Guillain-Barré Syndrome (GBS), vision impairment, and a neurological disorder known as acute disseminated encephalomyelitis (ADEM). All of these are important as they can have life-changing consequences to those who contract Zika.
The second direction involves focusing on therapeutics and a vaccine. This route has significant advantages as it focuses on taking out the virus before it has a chance to cause disease. But this direction requires far more resources as lab work would quickly have to turn into clinical trials. Only a few projects would be funded.
There is, however, one possible option for research to merge these two streams. It’s a protein known as NS1, for non-structural protein 1. It hasn’t gained significant attention in the media or the scientific literature for that matter. However, based on our knowledge from Zika’s close relative, dengue virus, this may be the lynchpin of Zika virus infection. With focused work on this protein, we may understand its pathogenesis, prevent secondary effects through new therapeutics, and possibly develop a vaccine.
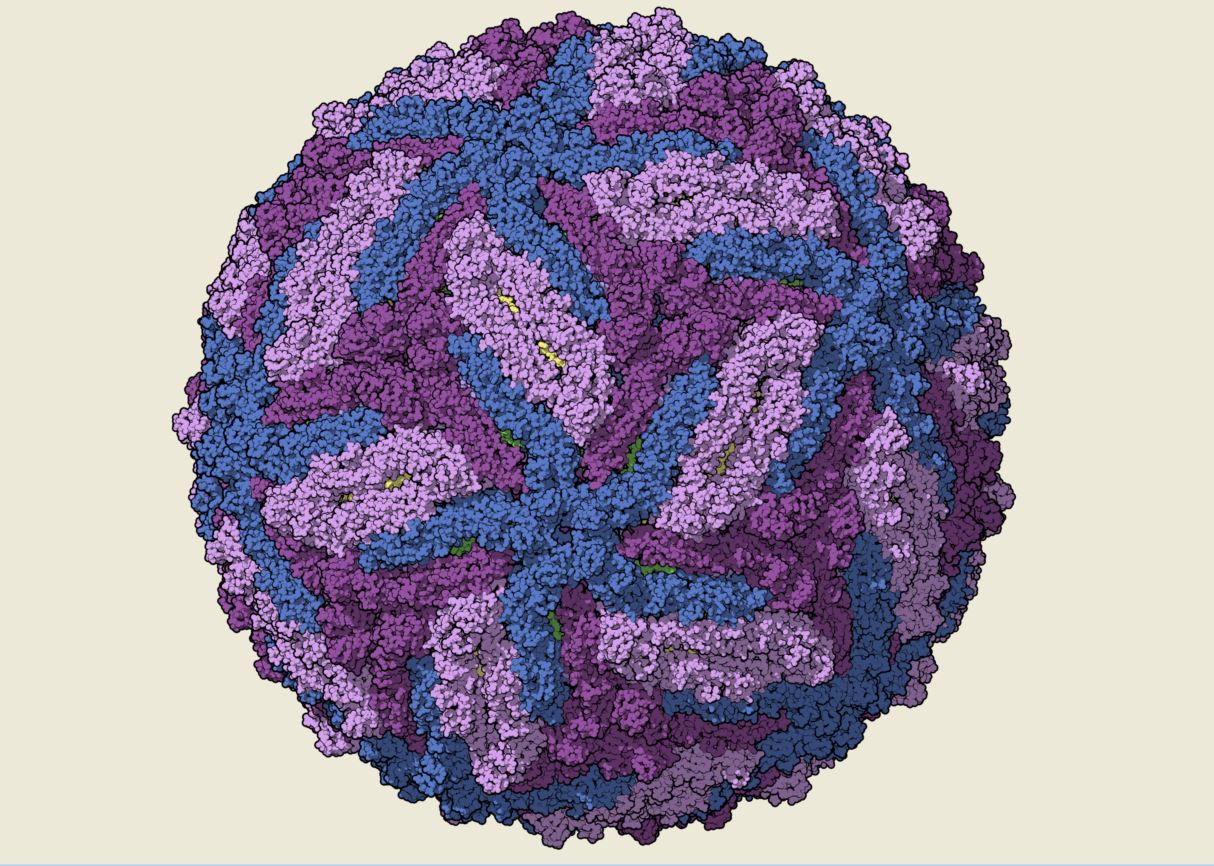
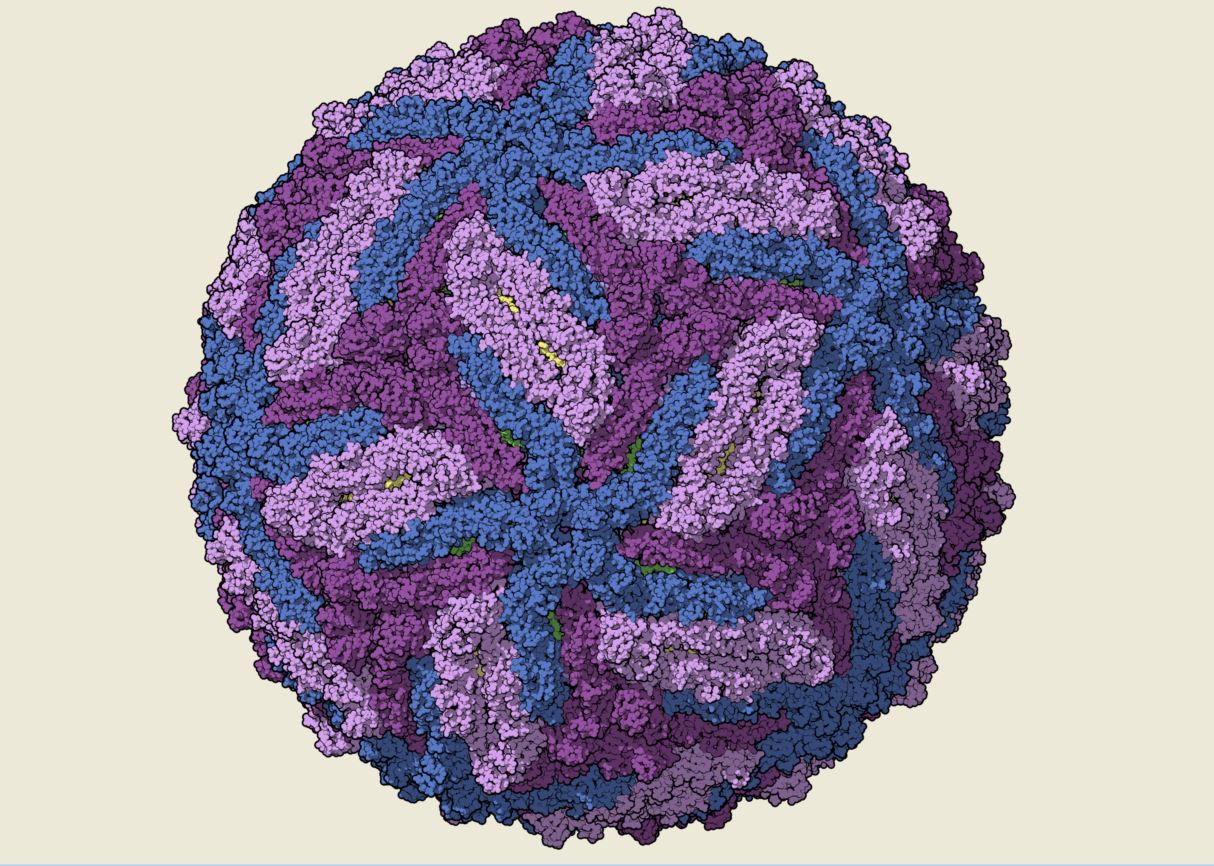
The NS1 protein in flaviviruses, which include Dengue, West Nile, and Zika, is a jack of all trades. It comes in three forms, a single protein, a dimer, and also a hexameric entity. Depending on the form and the location, a variety of functions are mediated ranging from viral survival to immune evasion.

The monomer and dimer forms are needed for viral replication. The monomer is able to acquire sugar molecules, giving it a unique look inside the cell. Once this has occurred, the protein dimerizes and becomes a regulator of RNA synthesis in combination with another viral protein, NS4. Without the monomer or dimer versions, a virus cannot survive in the cell. Moreover, the amount of virus produced in the cell may be changed with mutations in NS1.
The hexamer has a number of functions, all of which make the situation worse for the sufferer. The protein complex is secreted from the cell and can interact with various components of the body including the immune system. Although the entire picture isn’t complete, what is known suggests this form of NS1 is a major problem.
The first role of the complex is to disrupt the immune system. The protein can stall one of the most important antiviral activities, the complement system, by binding and hiding one of the factors necessary in activation of this process. This essentially slows down the defenses giving the virus more time to infect.
The hexamer can also stimulate inflammation, creating damage to blood vessels and destabilizing the barriers between the bloodstream and other areas such as the nervous system and the fetus. This could allow the virus to travel to these areas and increase the chances for secondary effects such as microcephaly, GBS and ADEM.
Finally, the complex acts as a decoy by protecting the virus from antibodies. The protein complex is covered in regions recognized by antibodies and can keep them from targeting the virus for destruction. In addition, this decoy mechanism can lead to a condition known as antibody-dependent enhancement (ADE), in which the antibodies accidentally allow infective viruses to gain access to immune cells. This can greatly worsen infection and offers another route for the virus to travel inside the body.
Not surprisingly, when it comes to developing a therapeutic or a vaccine, NS1 seems to be at the top of the list. Inhibition of this protein has been regarded as a prime route to help those suffering from dengue virus. It can help to reduce the likelihood of immune evasion and may also prevent ADE. The potential for vaccination based on NS1 also has been eyed for decades in terms of dengue virus and other flaviviruses such as yellow fever virus and Japanese Encephalitis.
In the context of Zika virus, little is known about NS1 in terms of its role in disease. However, there are clues providing some perspective. Based on this information, this protein may indeed be the perfect target for research and associated funding.
Analysis of the protein has shown changes in the NS1 protein have occurred between the relatively benign version of the virus, the African lineage, and the one now circulating in the Americas, known as the Asian lineage. In addition, these changes have been shown to be associated with higher amounts of virus in the body. This has been seen in clinical cases where the levels of Zika virus in fetuses have been up to 10,000 times higher than expected.
Considering the information already gained from other flaviviruses, there is reason to believe NS1 is indeed that central actor. The protein can lead to higher viral loads, an increase in attacks on the immune system, and higher levels of spread through the body, including the fetus. This in turn can increase the likelihood of the secondary effects.
There is another reason why an emphasis on NS1 may be a valuable direction. Because of the focus on this protein in other flaviviruses, the path to therapy and vaccine development may be shorter. By learning more about the Zika version of the protein, we can find similarities between this virus and its relatives and then use or alter current therapeutic agents in enough time to deal with this current wave.
Deciding on where funding for Zika-related research is not going to be an easy process and assuredly, more people will be upset than happy with the decisions. But in the context of public health and security, looking at NS1 as a priority may be the best option to deal with the situation. If this direction will allow researchers to deal with both pathogenesis and therapeutics, it should be at least given significant and serious consideration.
