This article was originally featured on The Conversation.
An early April 2023 decision by a U.S. district judge in Texas to reverse 23 years of approval of the abortion pill mifepristone has sparked explosive debate.
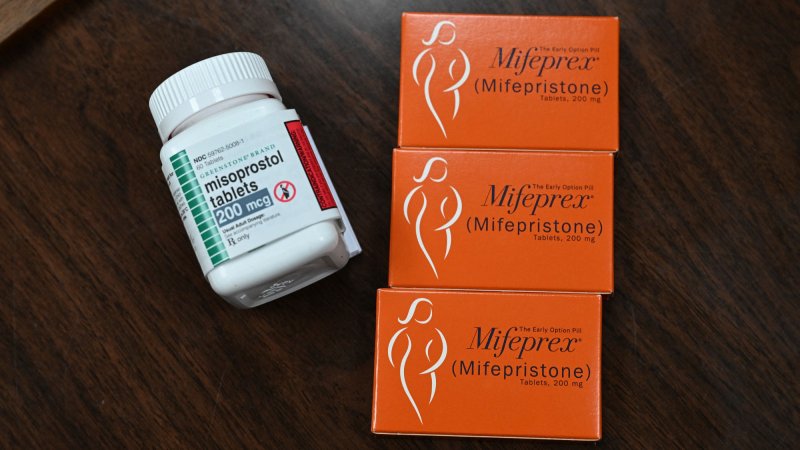
Mifepristone is a medicine that blocks the receptors for the hormone progesterone, which is needed for fetal development. It is part of a two-step medication abortion regimen along with misoprostol, a drug used to prevent stomach ulcers that also causes uterine contractions. Medication abortion with this two-step approach or a slightly less effective misoprostol-only regimen is now used in more than half of all abortions in the U.S.
The Food and Drug Administration approved mifepristone in the year 2000 for use in medication abortion up to seven weeks. Along with the approval, the FDA also required an in-person visit as an additional safety measure. In 2016 the FDA expanded its approval of mifepristone use for up to 10 weeks of pregnancy.
In January 2023, the FDA further modified its rules in light of many studies that show mifepristone is a very safe medication. It decided to not enforce the requirement for an in-person visit, allowing the drug to be offered by certified pharmacies with a prescription.
The Texas judgment by U.S. District Judge Matthew J. Kacsmaryk overturning the FDA’s approval would have taken this medication off the market altogether in the United States. The 5th U.S. Circuit Court of Appeals quickly responded, saying on April 12, 2023, that the plaintiffs could not challenge the original FDA approval of mifepristone because it is too late.
However, the 5th Circuit agreed with the plaintiffs that the FDA’s 2016 approval of mifepristone up to 10 weeks after pregnancy was invalid. In addition, drawing on an 1873 law, the Comstock Act, both the Texas district court and the appeals court said that mifepristone can no longer be sent through the mail.
In order to render these decisions, the Texas judge and the appellate court had to first determine that the groups that brought the case were harmed by the FDA’s original approval and thus had what is called, in legal terms, “standing” to be allowed to sue. The plaintiffs include a coalition of anti-abortion doctors’ associations that brought the lawsuit in Texas so that it would be assigned to this judge, who was an anti-abortion advocate before his judicial appointment.
This case, and another in which a federal judge from Washington made a different decision about mifepristone, are now headed to the Supreme Court. But regardless of how that court rules, we – a legal scholar and an academic obstetrician/gynecologist and complex family planning specialist – see multiple assertions about mifepristone in the decisions with potential ripple effects on reproductive health care and law.

Legal history paved the way
Both decisions stem from decades of judicial rulings that interpret medical science for legal ends. The 2022 Dobbs decision that overturned nearly 50 years of the constitutional right to an abortion opened the door for legal challenges to any and all abortions. Dobbs addressed medical care related to pregnancy and birth, but the case mainly focused on reinterpreting the legal history of abortion to justify overturning precedent.
While some states have further limited access to abortion in the wake of the Dobbs decision, they have not been able to successfully stop the distribution of medications that can induce abortions. In part, this is because both the FDA and the Department of Justice have allowed medication that induces abortion to be mailed from states where there are fewer legal restrictions.
The Texas case illustrates how judges apply their own reading of science to a thorny political question. Kacsmaryk’s reasoning echoes Justice Anthony Kennedy’s approach in a Supreme Court case known as the Carhart decision, which restricted doctors from performing a second-trimester abortion procedure.
In that 2007 case, Kennedy asserted that women experience psychological harms from having an abortion. Yet scientific studies show that the harm of denying an abortion and forcing women to birth are greater and longer lasting, with higher rates of death. Law influences public discourse, and these statements about psychological harms are now commonplace in anti-abortion communications. These arguments were central to the Texas judge’s critique of the FDA’s scientific process.
Assessing harms
Before asserting that the FDA’s scientific determination was inadequate, Kacsmaryk and the 5th Circuit appellate court had to decide whether the plaintiffs have standing to sue. The plaintiff doctors’ first standing argument includes the statement that they are harmed because they may, in the future, have to care for a woman who has an exceedingly rare complication from mifepristone prescribed by another doctor.
Potential harm does not align with long-standing principles related to judicial standing; the plaintiffs must show that the agency rule will harm them.
The decision on standing relies on a highly questionable interpretation of scientific evidence of harm. The 5th Circuit uses statistics about complications from medical abortions since 2000 to suggest that at least one doctor in the plaintiff’s associations, which they claim include approximately 8,200 medical professionals, will see a patient seeking emergency care for using mifepristone. Yet it cites no evidence – because there is none – that mifepristone alone causes complications. Further, it cites no evidence that access to mifepristone through the mail, or up to 10 weeks of pregnancy, increased the rate of complications.
The 5th Circuit that affirmed Kacsmaryk’s decision about standing claims this is a narrow decision about the harm to plaintiffs. The court said these doctors have standing because complications from medical abortion are statistically likely, that the FDA cut doctors out of the process of dispensing mifepristone, and that providing care to women who took mifepristone is emotionally draining for the doctors.

Flawed arguments
The Supreme Court has recently struggled to balance the overall impacts – burdens and benefits – of various regulations, such as student debt relief and immigration policies.
In this case, and using the doctors’ own theory of harm, there are actually numerous benefits that the plaintiff doctors receive from having mifepristone available to pregnant people in Texas. Those who cannot access mifepristone will have to either use less effective medication regimens or will be forced to get surgical abortions at later gestational ages. Delays means the fetus continues to grow, a fact about abortion access restrictions that deeply troubled Justice Kennedy.
All the risks associated with medical abortion – and therefore the time and resources doctors must spend caring for patients – will be higher if pregnant people are compelled to have surgical abortions or to give birth.
Judge Kacsmaryk frames the decision as one designed to protect women and girls, yet mifepristone is a drug that has more benefits than just safe abortion. It has been shown in numerous studies to help women safely treat an incomplete miscarriage and is now used off label for this purpose. Studies have also shown mifepristone to be helpful with labor induction, increasing the safety of the delivery process for someone who does continue with a pregnancy. Ongoing research into other applications for mifepristone may be interrupted by these judges’ decisions that limit the ways the drug can be used.
Finally, it is difficult to see how the FDA’s approvals of other medications are not vulnerable. For example, COVID-19 vaccines do not require an in-person doctor’s visit. Doctors who have been vocally opposed to the COVID-19 vaccine can easily find information to support arguments that they will have to care for vaccine injuries.
Doctors opposed to vaccines and other medications could also claim that it is too emotionally draining to treat patients who need their care – and therefore prevent other doctors who do not find it too emotionally draining from doing that important work for people who need medical care.
The legal and medical implications make clear just how much is at stake in these abortion-related decisions.![]()
Jamie Rowen is an associate professor of legal studies and political science at UMass Amherst. Jamie Rowen receives funding from National Science Foundation and Humanity United. Tami S. Rowen is an associate professor of obstetrics, gynecology and gynecologic surgery at University of California, San Francisco.
This article is republished from The Conversation under a Creative Commons license. Read the original article.