Last week members of the British House of Commons passed a bill legalizing mitochondrial DNA transfers–a process that combines three different sets of DNA to create an embryo. That means one day, it could be possible for children in the United Kingdom to have DNA from three parents.
Although the bill cleared the Commons by a vote of 382-128, it needs approval from the House of Lords before it can be enacted. Even with overwhelming government support, however, debate about the procedure is far from over.
Supporters argue there’s a need for three-person in vitro fertilization: Mothers can pass along potentially life-threatening diseases through their mitochondrial DNA. Mitochondria are the powerhouses of cells, and they contain their own set of DNA with 37 genes. Once a sperm fertilizes an egg, the father’s mitochondrion dissolve and the mother’s mitochondrial DNA sticks around. Mitochondrial DNA doesn’t carry information about specific traits–all of that information comes from the nucleus. Yet when a mother passes abnormal mitochondrial DNA on to her baby, the child can have problems generating enough energy in his or her cells. So, swapping out unhealthy mitochondria could prevent deadly mitochondrial diseases such as heart, kidney, and liver failure, as well as muscular dystrophy.
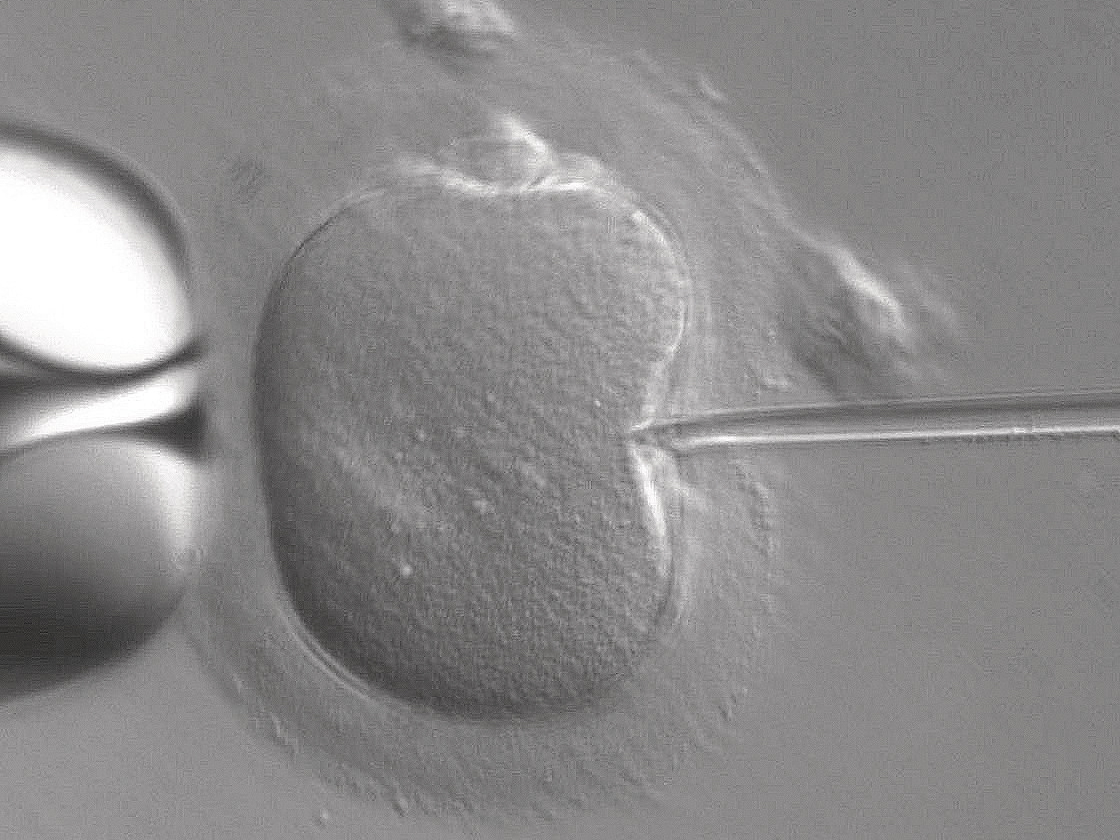
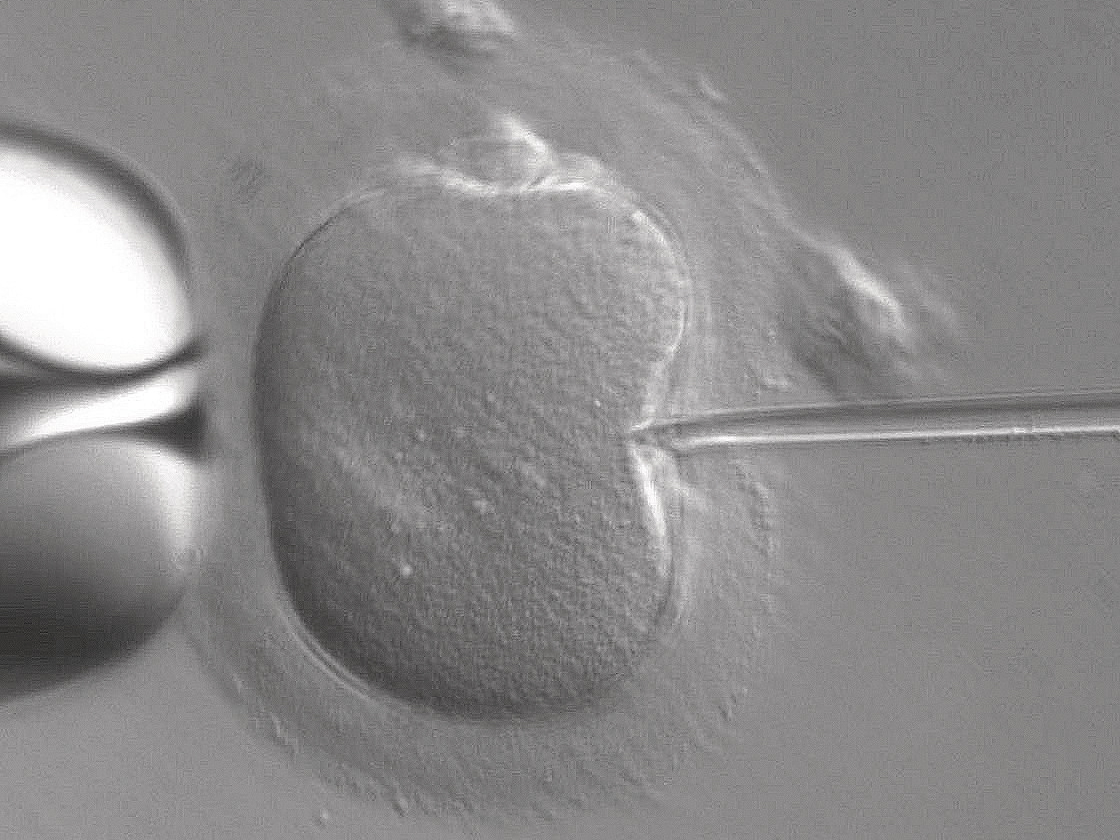
There are two ways to carry out that process with three-parent IVF, both of which involve a father, a mother with abnormal mitochondrial DNA, and a healthy female donor. In the first method, scientists take an unfertilized egg from the mother and scoop out its nucleus, which contains almost all of the important genetic information for a child (except those related to mitochondria). They then place this nucleus in the female donor’s unfertilized egg, which has had its nucleic DNA removed. Combining the first mother’s nucleus with the donor’s healthy mitochondria keeps the embryo from inheriting any mitochondrial diseases. The scientists then fertilize the combined egg with the intended dad’s sperm, creating a healthy embryo.
The second method is similar but more complicated. Scientists swap nuclei after both the mother’s eggs and donor’s eggs have been fertilized (the mother’s by the father’s sperm, and the donor’s by a donated sperm). The scientists discard the donor egg’s nuclei and put the mother-father nuclei into the donor’s egg. This newly combined embryo is the only one to mature.
If you’re confused, don’t fret; here are some detailed diagrams showing how the two processes work:


Because of how new the procedures are and the way they tamper with the fertilization process, many groups aren’t too happy about the idea of three-parent IVF. Even so, genetically modifying embryos brings about ethical questions, such whether this would set a precedent for other modifications.
Slippery slope toward “designer” babies?
Some British interest groups have expressed concern about the potential for in vitro fertilized eggs that are genetically engineered to have, for example, blonde hair, more intelligence, mor increased athleticism. The Human Genetics Alert took an ethical stance against mitochondrial transfers, because they say it will “inevitably lead to a future of ‘designer babies‘.” Experts we spoke to, however, aren’t convinced the leap from mitochondrial transfer to genetic trait modification is so direct.
“The intention here is purely therapeutic,” says David DeGrazia, a philosophy professor at George Washington University who specializes in bioethics. “It’s to avoid certain diseases an embryo and then a baby can have as a result of mitochondria. Mitochondria don’t have anything to do with the characteristics that might be sought in a designer babies.”
The “slippery slope” concept usually applies to any new, ethically questionable medical procedures. The idea is that science is automatically going to keep pushing ahead with no checks on how far it goes. But that’s not always the case, says Lisa Campo-Engelstein, a professor of bioethics and obstetrics & gynecology at the Albany Medical College. “We can put limits on [the procedure], but we have to be willing to do so.”
Destruction of embryos
The Catholic Church in England and Wales view the procedure as destructive to the embryos.
“It’s hard to argue against religious beliefs,” Campo-Engelstein says. That’s because the definition of life differs from person to person, and the concept of when a person begins to have a soul enters a less scientific discussion.
Conservative parliament member Fiona Bruce, who led the opposition to the bill, said, “One of these procedures we are asked to approve today, pronuclear transfer, involves the deliberate creation and destruction of at least two human embryos, and probably in practice many more, in order to create a third embryo which it is hoped will be free from human mitochondrial disease. Are we happy to sacrifice two early human lives to make a third?”
DeGrazia says it’s confusing for Bruce to say two lives are destroyed to create a third one. To him, the only thing that’s lost is the nuclei from the mitochondrial donor egg. “Look, the embryo created by the donor egg, that sort of sacrifice, I can understand that point,” he says. “I don’t agree, but I understand it.”
Safety first
Bruce also mentioned on the day the bill passed the Commons her concerns about the safety of the procedure, in addition to the ethical doubts. This is a point on which most bioethicists agree: Safety and efficacy of the treatment must be proven before it gains approval.
In a recent panel assessment of three-parent IVF, the U.K.’s Human Fertilization and Embryology Authority wrote that while moving medical procedures from research to practice has a “degree of uncertainty,” it remained certain that the processes are not unsafe based on available evidence. The HFEA cites a number of studies at the end of its assessment pointing to the overall safety and efficacy of the procedures. But so far the two methods are known to work only with mice, monkeys, and human eggs that have not been implanted back into the uterus, according to Newcastle University. British doctors need the okay from the government before they can implant the embryos into humans.
Bonnie Steinbock, a philosophy professor at the University of Albany, says a major sticking point is the need for the procedure. Steinbock participated in a U.S. Federal Drug and Administration panel as an ethics expert in February 2014, during which doctors raised questions about mitochondrial transfer. They wondered: Why invest time and resources to study this treatment, or run the risk of bad outcomes, when you can just use a donor egg? The reason, she says, is that mothers with faulty mitochondria find it important to have a genetic connection to their kid. “They want the baby they would have had, but for their infertility,” says Steinbock.
Will the U.S. be next to approve?
Campo-Engelstein says she’s confident in the U.K.’s steps toward approving three-parent IVF, because the country’s better about regulating medical practices than the United States. She notes that America is more like the “Wild West” of experimental fertility treatments. “Whatever you want to do, you can go for it,” she says. In the U.S., patients are allowed to take part in human clinical trials of a treatment before the FDA approves it. As it stands now, the U.K. does not allow for mitochondrial transfers in humans, not even for clinical trials, unless the most recent legislation passes.
Meanwhile, reproductive practices such as ovarian transplantation and egg preservation have become popular in the U.S., even without official FDA approval. But because they aren’t regulated, the procedures become cost prohibitive, often costing patients thousands of dollars out-of-pocket. Even if the mitochondrial transfer procedures caught on in the U.S. experimentally, they might also come at a high cost to patients until the procedure gains FDA approval (if that even happens).
