In the wake of mass casualty events like shootings, blood centers are among the first lines of defense against fatalities. Trained staff at these facilities collect blood from donors year-round, clean and process it, and then distribute it to regional hospitals and first responders on request. Following storms and other emergencies, they might circulate supplies across the country to help depleted centers keep up with demand. That’s why they need a stockpile of donations before disasters break out—and a steady stream after to replenish the stores.
Blood banks can be especially critical for trauma cases. In most metropolitan areas, it takes about 30 minutes from the time of the 911 call to get an injured individual to a hospital, says CJ Winckler, an emergency medicine doctor at UT Health San Antonio and deputy medical director for the San Antonio Fire Department. Within that time, the patient can lose several pints of blood (on average, adults hold 1.5 to 2 gallons of the stuff). If their oxygen supply runs too low, they can go into hemorrhagic shock.
EMS workers have a few ways of sustaining a person’s vitals—but ultimately, what the patient needs is more blood. “If they’re hemorrhaging, they should receive a transfusion as soon as possible,” Winckler says. If the ambulance already has a cooler of donated blood, the medics can get the process started right away. Once the individual reaches the ER or trauma ward, they could require dozens of additional units, aka pints, depending on their size and the scope of the injury.
[Related: A new AT&T update could make 911 calls more effective]
In sum, when a crisis emerges, hospitals and first responders need immediate access to loads of blood. And the best way to ensure they’re prepared is by donating on a regular basis, says Adrienne Mendoza, COO of the South Texas Blood & Tissue Center. When a gunman killed 21 teachers and students at Robb Elementary School on May 24 and injured many others, her team had 15 units of whole blood—as opposed to blood broken down into plasma, platelets, and cells—ready to fly to the scene. “We got the call around noon on Tuesday that something was happening in Uvalde,” she explains. “An air ambulance came by to pick up the units. Then we sent 10 units of O-negative red blood cells for pediatric patients at Uvalde Memorial Hospital.”
Those resources were available at a moment’s notice because of regular blood donors around the region. (Mendoza’s center has a program called Brothers in Arms that motivates Texans to contribute O-positive blood to store in ambulances, fire trucks, helicopters, and ERs.) But once they used up their cache of units, the staff at South Texas Blood & Tissue had to turn to their local and national networks.
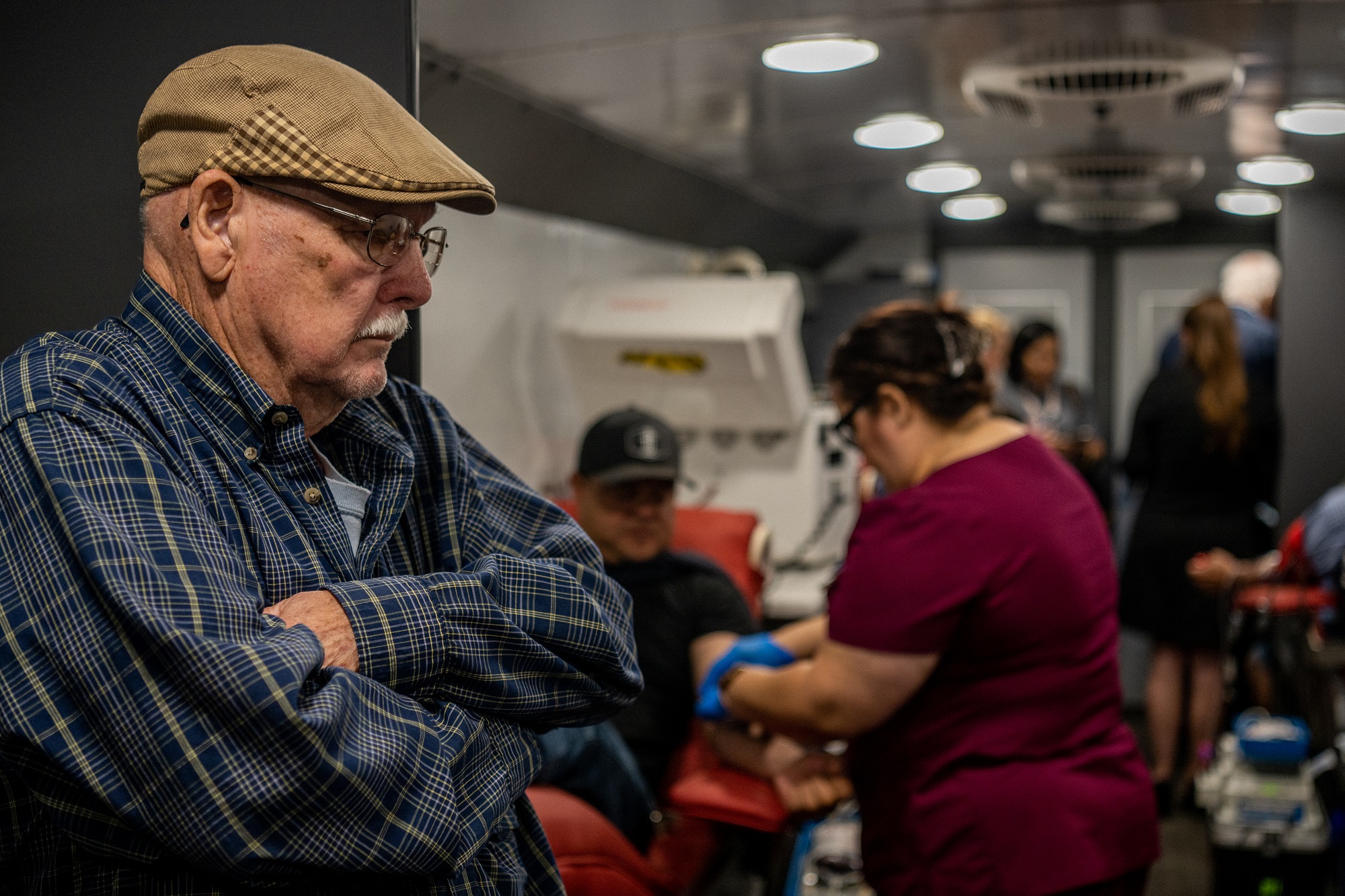
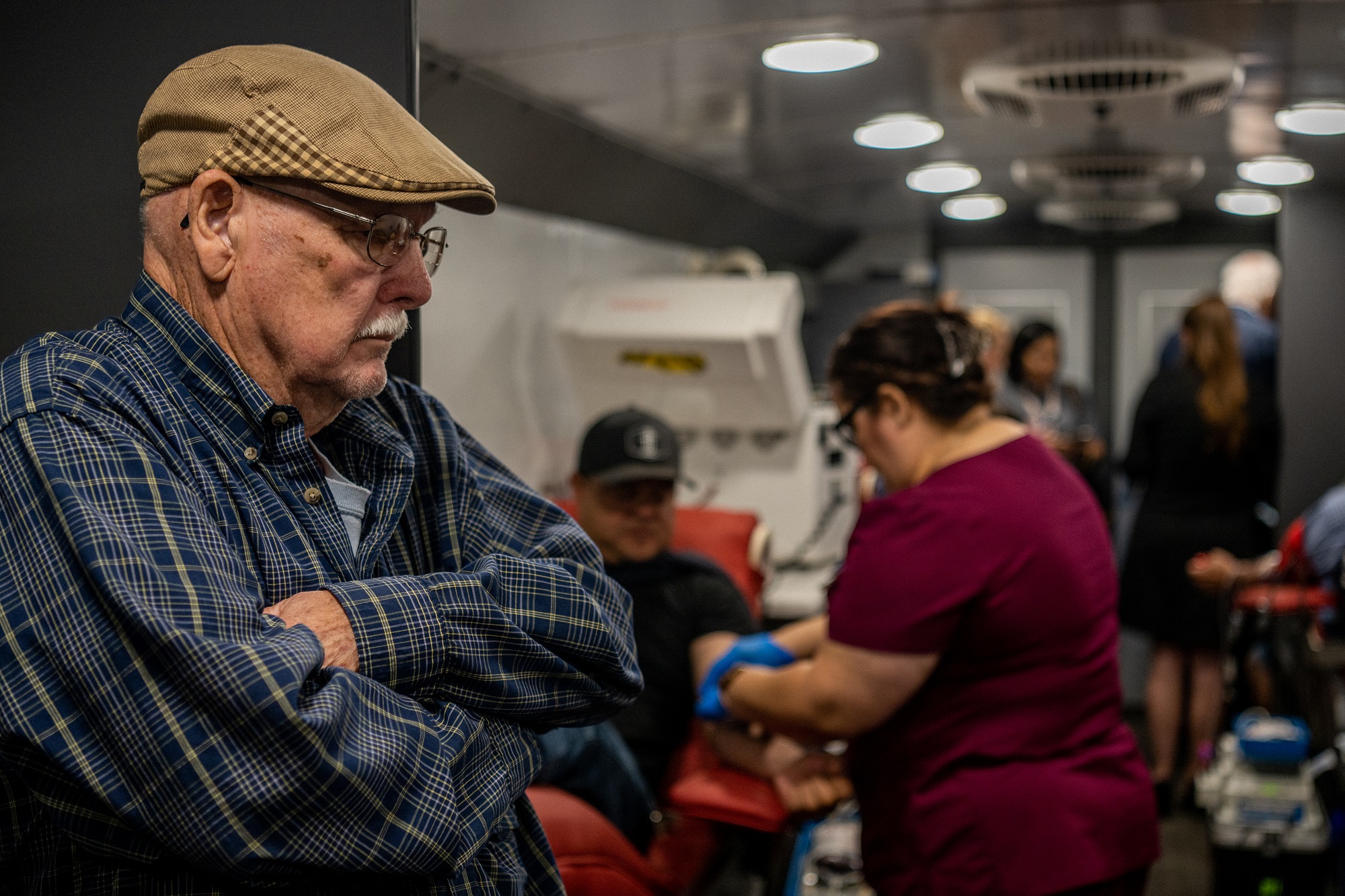
“We’ve had a record number of [walk-in] donations this week,” Mendoza says. “During a good day in the pandemic, we would see about 400 people.” On May 25, the center had 1,100 donors lined up at its eight locations around San Antonio.
Mendoza’s team is also part of Blood Emergency Readiness Corps, a group that was founded in late 2021 in response to the US donor shortage—and the country’s uptick in gun violence. The corps includes blood centers in 37 states and allows supplies to be quickly diverted to places in crisis. After the Uvalde shooting, organizations in Florida, Oklahoma, and from across the West Coast flew O-negative units over to South Texas Blood & Tissue’s central office. From there, they were shared with children undergoing surgery at two area trauma centers.
Another reason the region’s blood donation network mobilized so quickly is because it had gone through a similar scenario before. In 2017, a mass shooter killed 26 and wounded 22 churchgoers in Sutherland Springs, Texas, just northeast of San Antonio. “We built and planned for another large casualty event, and unfortunately, it happened,” Winckler says, referring to the tight chain between first responders, hospitals, blood centers, and donors in South Texas.
[Related: Everything you’ve ever wanted to know about donating bone marrow]
While the demand for blood donors will stay high around Uvalde, people across the country should know they can help, too. Even if their blood doesn’t make it directly to the shooting survivors, it will undeniably be used to heal other sick individuals, like premature babies and sickle cell anemia patients. “Everywhere a donor gives, that blood’s going to find a taker,” Mendoza says. “Trauma cases take up a lot of units and can deplete local supplies quickly, but they only account for 3 percent of the need. A lot of people need blood every single day: It’s life-saving and an emergency for them.”
She points out that if every eligible American donated blood four times a year, the country “would never see a shortage.” But at the moment, only 3 percent of the population is giving at a blood center, mobile unit, or drive annually.
Susan Forbes, a senior vice president at OneBlood, which runs a network of donation centers across Florida, offers similar advice. “It’s so important that people be proactive about being a donor,” she says. “We went through two mass tragedies in the past six years here, with the Pulse and Parkland shootings. The blood supply on the shelves played a role in saving the victims. Don’t wait for a tragedy. It’s the donor who gave yesterday who will make an impact.”
