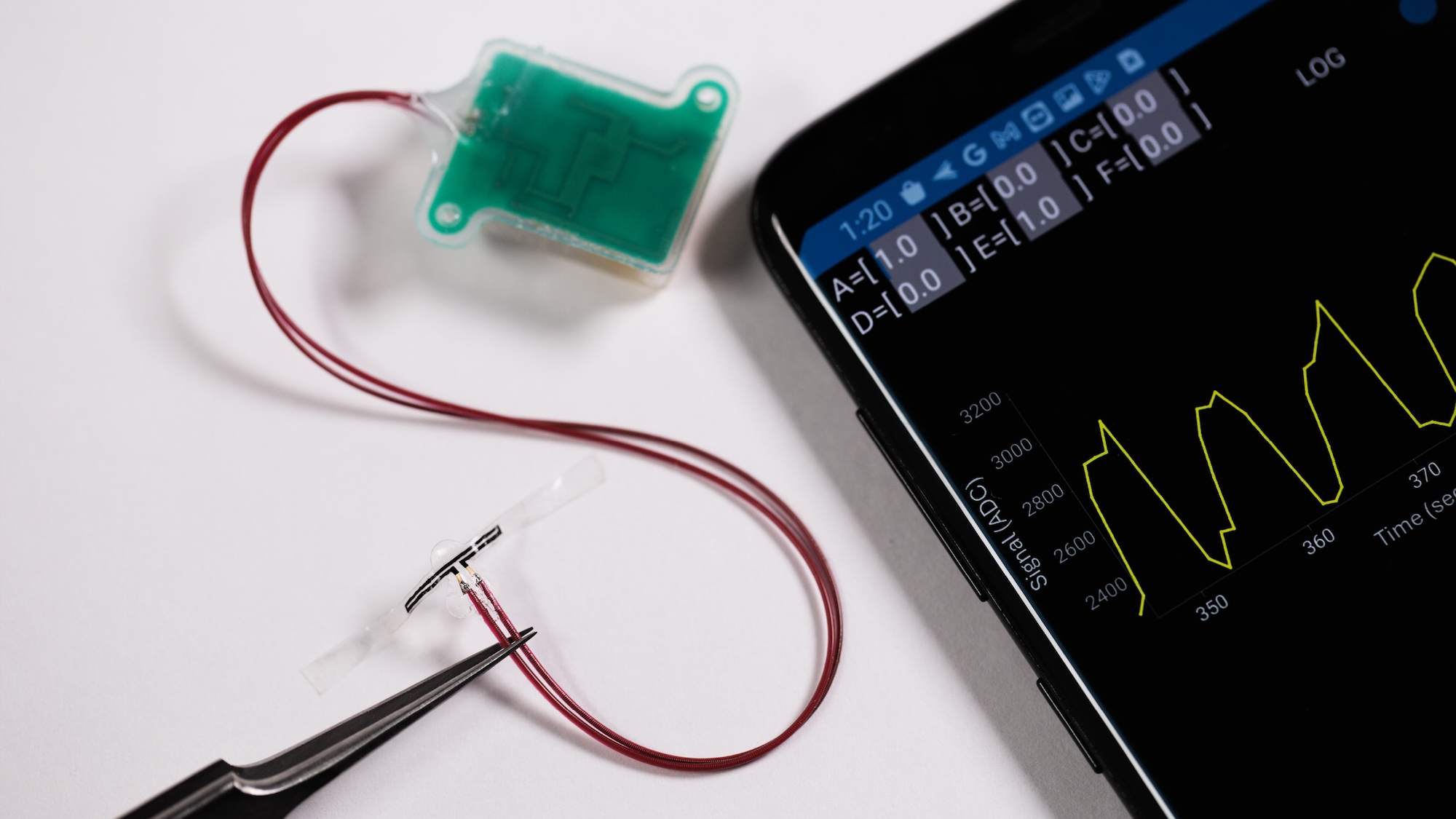
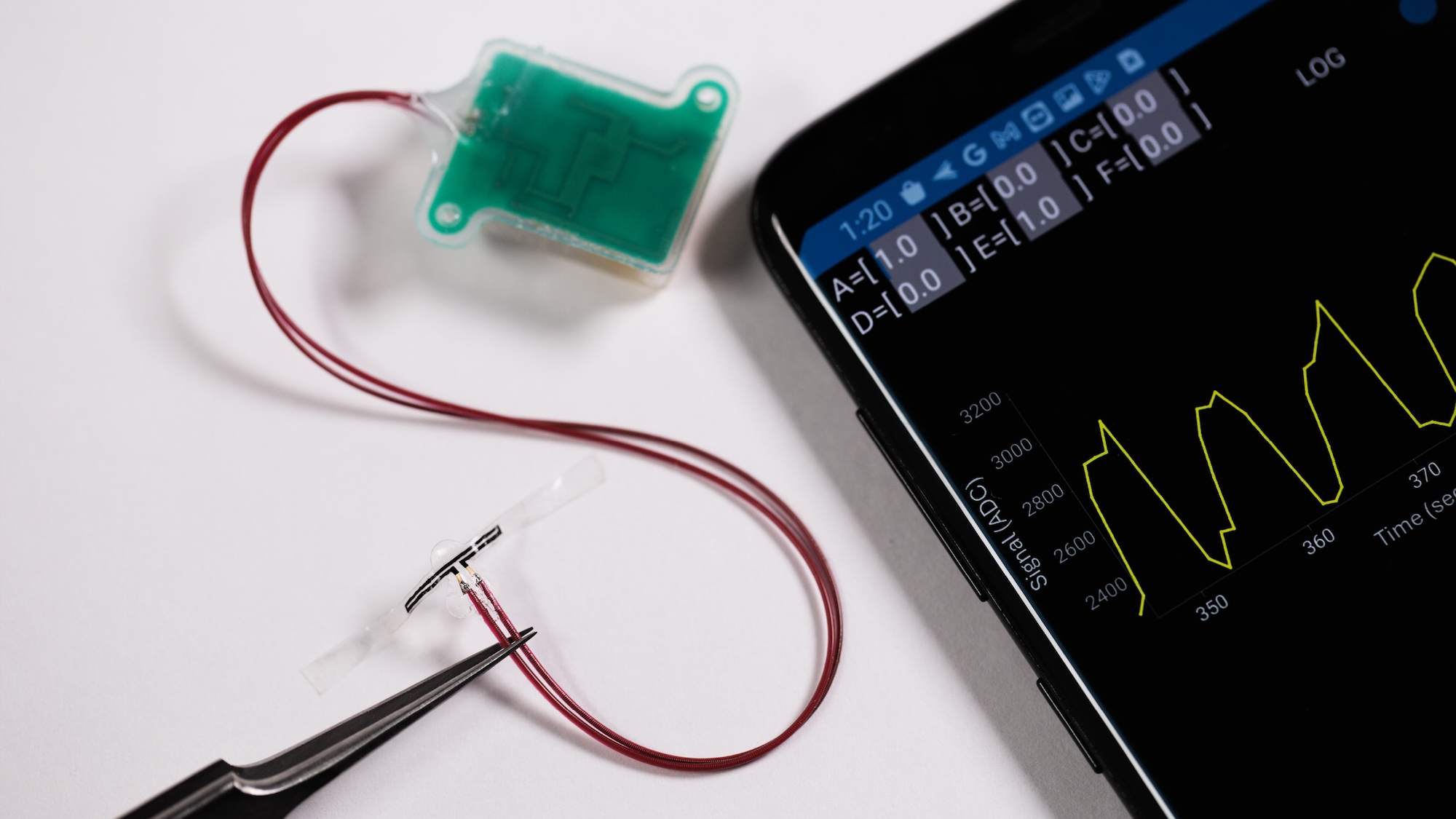
For people dealing with spina bifida, paralysis, and various bladder diseases, determining when to take a bathroom break can be an issue. To help ease the frequent stress, researchers at Northwestern University have designed a sensor array that attaches to the bladder’s exterior wall, enabling it to detect its fullness in real time. Using embedded Bluetooth technology, the device then transmits its data to a smartphone app, allowing users to monitor their bodily functions without far less discomfort and guesswork.
The new tool, detailed in a study published today in the Proceedings of the National Academy of Sciences (PNAS), isn’t only meant to prevent incontinence issues. Lacking an ability to feel bladder fullness extends far beyond the obvious inconveniences—for millions of Americans dealing with bladder dysfunctions, not knowing when to go to the bathroom can cause additional organ damage such as regular infections and kidney damage. To combat these issues, the new medical device mirrors the bladder’s own elasticity.
[Related: This drug-delivery soft robot may help solve medical implants’ scar tissue problem.]
“The key advance here is in the development of super soft, ultrathin, stretchable strain gauges that can gently wrap the outside surface of the bladder, without imposing any mechanical constraints on the natural filling and voiding behaviors,” John Rogers, study co-lead and professor of material sciences and biomedical engineering at Northwestern University, said in a statement.
As a bladder fills with urine, its expansion stretches out the sensor material, which in turn wirelessly sends data to a patient’s smartphone app. This also works as the organ contracts after urination, providing users with the real-time data throughout the day’s ebbs and flows. In small animal lab tests, the battery-free device could accurately monitor a bladder for 30 days, while the implant lasted in non-human primates as long as 8 weeks.
“Depending on the use case, we can design the technology to reside permanently inside the body or to harmlessly dissolve after the patient has made a full recovery,” regenerative engineer and study co-lead Guillermo Ameer said on Monday.
Researchers believe their device could reduce the need for uncomfortable, infection-prone catheters, as well as limiting the use of more invasive, in-patient bladder monitoring procedures. But why stop there?
The team is also testing a separate, biodegradable “patch” using a patient’s own stem cells. Called a pro-regenerative scaffold (PRS), the new material also expands and contracts alongside the bladder’s movements while encouraging the growth of new organ cells. New tissue remains in place as the patch dissolves, allowing for faster, more effective healing possibilities. Researchers hope to one day combine their PRS work alongside their wireless monitoring sensors.
“This work brings us closer to the reality of smart regenerative systems, which are implantable pro-regenerative devices capable of probing their microenvironment, wirelessly reporting those findings outside the body… and enabling on-demand or programmed responses to change course and improve device performance or safety,” said Ameer.
For even more restored functionality, the team believes their sensors could eventually incorporate additional technology to stimulate urination on demand using the smartphone app. Taken as a whole, the trio of medical advances could one day offer a far less invasive, comfortable, and effective therapy for patients dealing with bladder issues.
