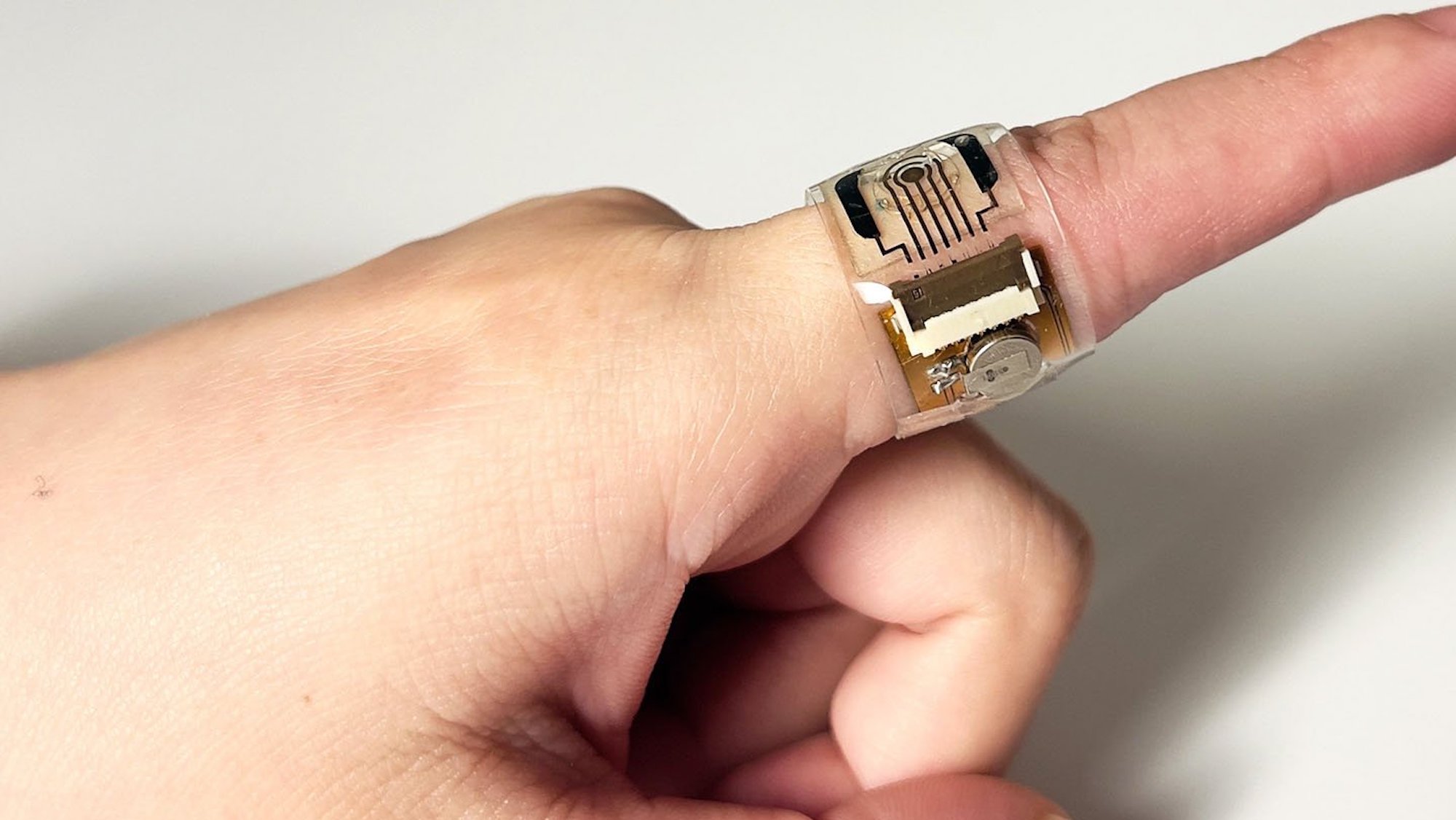
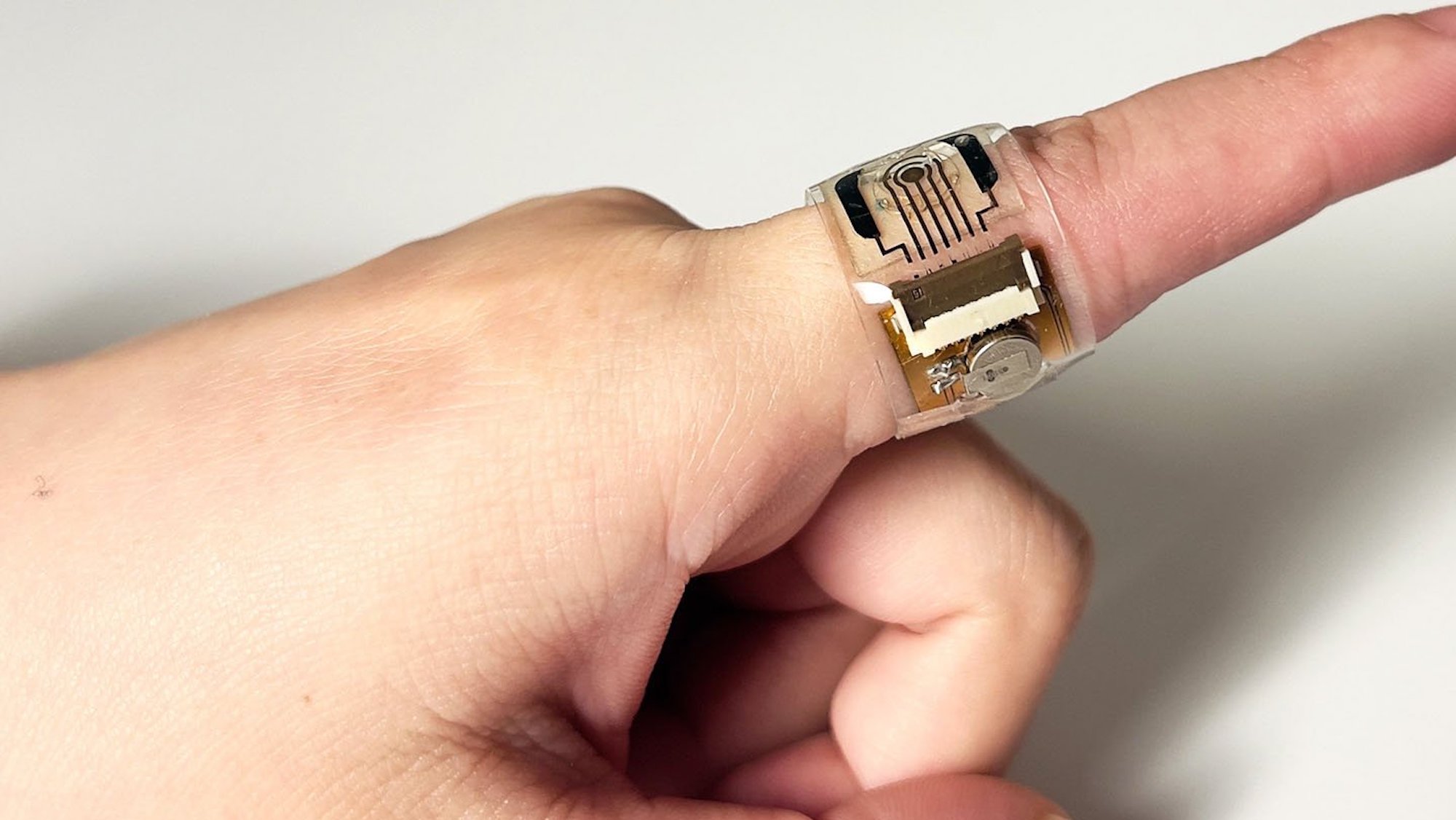
Wearable sensors can already monitor a variety of important health characteristics. But they are still far short when it comes to detecting hormonal levels, particularly for women. A new device designed by researchers at Caltech, however, is specifically tailored to measure one of women’s most vital and influential hormones. According to the team’s study, recently published in Nature Nanotechnology, their new wearable sensor can detect and assess users’ estradiol levels by just analyzing sweat droplets.
Estradiol, the most potent form of estrogen, is a crucial component in women’s health. Not only is it necessary in regulating reproductive cycles and ovulation, but this hormone’s levels are directly correlated to issues ranging from depression, to osteoporosis, to even heart disease. Currently, estradiol monitoring requires blood or urine samples collected either in-clinic or at-home. In contrast, Caltech’s new sensor, created by assistant professor of medical engineering Wei Gao, only needs miniscule amounts of sweat collected via extremely small automatic valves within its microfluidic system.
[Related: This organ-failure detector is thinner than a human hair.]
The sensor’s reliance on sweat to measure estradiol isn’t only impressive due to its non-invasive nature; according to Caltech’s announcement, the hormone is about 50 times less concentrated in sweat than in blood.
The wearable’s monitoring system utilizes aptamers—short, single-strand DNA capable of binding to target molecules like artificial antibodies. Gao’s team first attached aptamers to a surface imbued with inkjet-printed gold nanoparticles. The aptamers then could bind with targeted molecules—in this case, estradiol. Once connected, the molecule gets recaptured by other titanium carbide-coated gold nanoparticles known as “MXenes.” The resultant electrical signal can be wirelessly measured and correlated to estradiol levels via a simple-to-use smartphone app.
To actually collect the sweat samples, the sensor uses tiny channels controlled by automatic valves to allow only fixed amounts of fluid into the sensor. To take patients’ sweat composition differences into consideration, the device also consistently calibrates via information collected on salt levels, skin temperature, and sweat pH.
This isn’t Gao’s first sweat sensor, either—previous variants also could detect the stress hormone cortisol, COVID-19, as well as a biomarker that indicates inflammation.
“People often ask[ed] me if I could make the same kind of sweat sensor for female hormones, because we know how much those hormones impact women’s health,” Gao said via Caltech’s announcement. With further optimization, the new estradiol sensor could help users attempting to naturally or in vitro conceive children, as well as aid those necessitating hormone replacement therapies. According to Gao, the team also intends to expand the range of female hormones they can detect, including another ovulation-related variant, progesterone.
