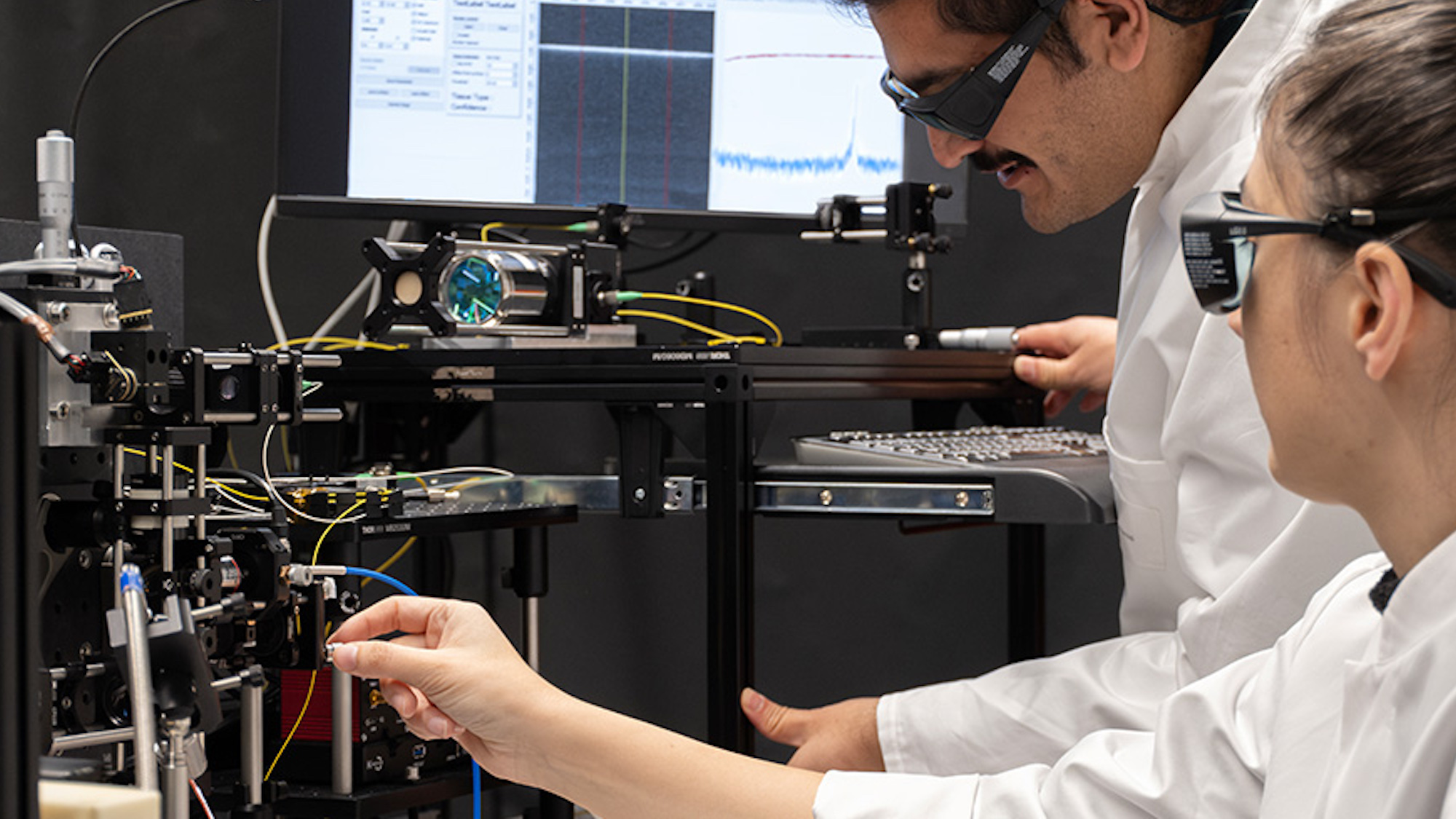
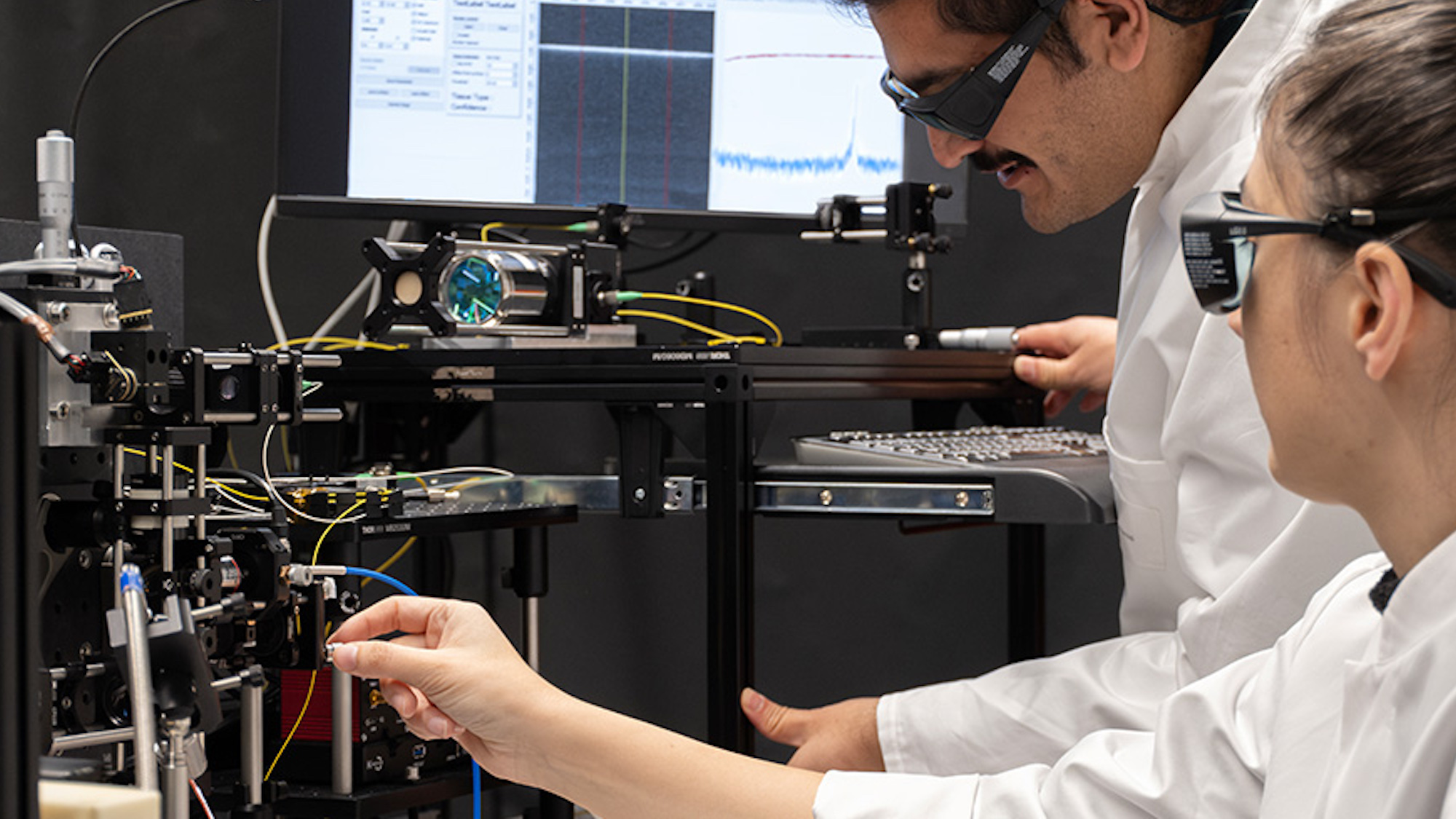
When it comes to slicing into bone, three lasers are better than one. At least, that’s the thinking behind a new, partially self-guided surgical system designed by a team at Switzerland’s University of Basel.
Although medical fields like ophthalmology have employed laser tools for decades, the technology’s applications still remain off the table for many surgical procedures. This is most frequently due to safety concerns, including the potential for lasers to injure surrounding tissues beyond the targeted area, as well as a surgeon’s lack of full control over incision depth. To potentially solve these issues, laser physicists and medical experts experimented with increasing the number of lasers used in a procedure, while also allowing the system to partly monitor itself. Their results are documented in a recent issue of Laser Surgeries in Medicine.
[Related: AI brain implant surgery helped a man regain feeling in his hand.]
It’s all about collaboration. The first laser scans a surgery site while emitting a pulsed beam to cut through tissue in miniscule increments at a time. As the tissues vaporize, a spectrometer analyzes and classifies the results using on-board memory to map the patient’s bone and soft tissue regions. From there, a second laser takes over to cut bone, but only where specifically mapped by its predecessor. Meanwhile, a third optical laser measures incisions in real-time to ensure the exact depth of cuts.
Using pig legs acquired from a nearby supplier, researchers determined their laser trifecta accurately performed the surgical assignments down to fractions of a millimeter, and nearly as fast as the standard methods in use today. What’s more, it did it all sans steady human hands.
“The special thing about our system is that it controls itself without human interference,” laser physicist Ferda Canbaz said in a University of Basel’s profile on December 5.
The system’s benefits extend further than simply getting the job done. The lasers’ smaller, extremely localized incisions could allow tissue to heal faster and reduce scarring in the long run. The precise cutting abilities also allow for shaping certain geometries that existing tools cannot accomplish. From a purely logistical standpoint, less physical interaction between surgeons and patients could also reduce risks of infections or similar postsurgical complications.
Researchers hope such intricate angling could one day enable bone implants to physically interlock with a patient’s existing bone, potentially even without needing bone cement. There might even come a time when similar laser arrays could not only identify tumors, but subsequently remove them with extremely minimal surrounding tissue injury.
