Launch the slideshow to see the tech behind today’s–and tomorrow’s–advanced prosthetics. Also, click here to learn how high-tech prosthetics help disabled athletes stay on top of their game.
There’s always a Plan C-West Point teaches you that. If the road is mined, the bridge in splinters, and your opponent’s brigade massing on your left, you find a new road, build a new bridge. That´s Army DNA, the building blocks of a successful warrior, and it has been flush through Capt. Dawn Halfaker´s cells since her first weeks at the elite military college and as a guard on its women´s basketball team. Keep moving. There´s always another way.
Then you graduate and, because you´re an action junkie thrilled by weapons and foreign cultures, you´re assigned to run a military police station outside Baghdad. One morning before sunrise in June 2004, you´re bumping along in a Humvee on a routine patrol when someone aims a rocket-propelled grenade your way. It´s a lucky shot. The bomb tunnels into the carriage, shears off your buddy´s arm, and blasts through your own, making spaghetti out of tendons and muscle. What the insurgents don´t get, the surgeons finish off, leaving you with nothing below your shattered right scapula but expectations.
You’re 24, a child of the computer age. When you wake up and learn there is no more right arm to write and eat and shoot jumpers with, you just know that the country that invented supercomputing and reconstructive surgery can give you something gleaming and spectacular. An arm to rival Will Smith´s appendage in I, Robot.
Since the invasions of Iraq and Afghanistan, more than 370 U.S. soldiers have had amputations. Indeed, there are wheelchair traffic jams on the third floor of Walter Reed Army Medical Center in Washington, D.C. That´s where Halfaker befriended Melissa Stockwell, a former gymnast and rock climber who was in Baghdad for only a few weeks before she lost her left leg to a roadside bomb in April 2004.
The two women bonded in frustration. Stockwell, 26, received the microprocessor-enhanced C-Leg but struggled for months to walk free of pain, wishing that the large silicone socket holding what she calls her “little leg” wouldn’t chafe or thrust to the side, broadcasting her limp. Halfaker was the lone female soldier with what’s bloodlessly called a shoulder disarticulation, her right side barren like a sheer cliff. Prosthetists fit her at first with a partly mechanical, partly battery-powered arm held on with a thick plastic socket that fit like a shield and was Velcroed around her body. The device worked with muscle power; when she shrugged, pulleys and cables would trigger the motorized arm to open a blocky claw. It was a prosthetic born out of a previous war, uncomfortable and clumsy, and made her feel like a Playskool toy-and she let the prosthetists know her displeasure. “I don’t want an arm that weighs 20 pounds. I want an arm that weighs three pounds,” she told them. Something that wouldn’t slow her down. She was offered a hand that was a hook, a device straight out of the post-World War II weepie The Best Years of Our Lives. Absolutely not. “Because,” Halfaker said, “it looks like a hook.”
And that was it. There was no Plan C. For Stockwell, there was no leg and socket that would allow her to stride quickly and pain-free, that didn’t leave raw, angry marks on her pale thigh. For Halfaker, there was no arm that was strong and nimble and light enough that she could slip it under a silk blouse. Stockwell persisted, learning to walk in her new mechanical leg, though with a noticeable limp. She adapted. Halfaker rebelled, left her arm in a heap in her room. She learned to wash, dress, drive, and run with one arm, her empty sleeve dangling by her side. She adapted too.
But one day soon, in part because of the experiences of Iraq veterans like Stockwell and Halfaker, prosthetics wearers won´t have to do so much adapting. It´s the prosthetics that will be doing the adapting.
Prosthetics´ Manhattan Project
Nothing about a prosthetics patient´s fake limbs is optimal-not their speed, mobility, comfort or looks. This is partially because the market, though steady, is small, and the funding to advance prosthetics technology doesn´t flow as heavily as it does in, say, cancer research. There are about 1.8 million amputees in the U.S-mostly elderly stroke and diabetes patients-but the number of prosthetics users is significantly lower. Another inhibiting factor, of course, is the tremendous challenge of mechanically replicating the movement and dexterity of human limbs, which are as dependent on two-way communication with the brain as they are on the strength of bone and muscle.
But Halfaker and Stockwell were injured at an auspicious moment in the country´s attitude toward the prevention and treatment of limb loss. The nationwide support organization Disabled American Veterans has been lobbying for improved care for aging veterans hobbled by back and hip pain aggravated by poor-fitting prosthetics. Meanwhile, in Iraq, Kevlar vests and slick battlefield surgical units have kept more wounded soldiers alive (even if with missing limbs) than during any previous war. Government officials, keenly aware of the shoddy treatment given injured Vietnam vets-who often waited months for prosthetics-have vowed that these young men and women would not be treated the same.
In addition to the best care available now, that promise has sparked serious investment in the future. Don´t just think sockets and computerized body extensions, scientists are being told. Collaborate across fields. Explore every angle-even the regenerative powers of salamanders [see “Salamander Secrets,” page 74]. In 2005 the Department of Veterans Affairs budgeted $7.2 million to create the Center for Restorative and Regenerative Medicine at the VA Medical Center in Providence, Rhode Island. This year the Defense Advanced Research Projects Agency-which has paid for everything from mine-hunting robotic lobsters to sleep-deprivation research-began funding two prosthetics projects for $48.5 million, hoping the teams will devise a stronger, more functional arm in two years and, in four years, a neurally-controlled arm with sensory capabilities and greater degrees of motion.
The ultimate goal: to create prosthetics that interact with the body, tapping directly into the brain´s desires and sending back progress reports. To do this, artificial limbs will need additional sensors to gather information on speed, angle, gait and balance. Improvements in metals, plastics and other materials will make prosthetics lighter, more flexible and more easily integrated onto the body. “It requires a kind of Manhattan Project” in terms of coordination and commitment, says prosthetics innovator Hugh Herr, director of the biomechatronics group at MIT´s Media Laboratory. Herr is a uniquely knowledgeable advocate for amputees, having worn two below-the-knee prosthetics for decades, since losing his legs to frostbite while ice climbing in New Hampshire as a teenager. “We’re at a time in history where there are many core technologies that are getting close,” he says. “And if there’s funding, there will be an opportunity for dramatic and profound innovation-what even Hollywood would view as bionics.”
Painstaking Progress
Before World War II, amputees wore static prosthetic attachments that were little better than peg legs. Then came complicated strap-, cable- and pulley-intensive mechanical arms, which opened a claw. By the 1960s, Soviet scientists had discovered that the amputee´s body has far more resources to call upon. Electrodes placed on the skin could detect a muscle´s myoelectric signals-its contractions-and transmit them to a battery-powered prosthetic, which would bend or straighten the arm. By the early 1980s, as the needs of injured Vietnam veterans spurred research, microprocessors allowed for gradations of movement and speed, rotation and flexion. Still, the stiff prosthetics make a series of many individual, sometimes jerky motions instead of executing seamlessly combined moves. The technology has advanced past the old myoelectric arms, which processed one signal at a time to move the elbow, wrist or hand. But even with simultaneous functioning of these controls, motions can be slow and require the wearer´s intense concentration. Simply doing dishes or getting dressed can be exhausting.
Prosthetic-leg wearers have seen more innovation than those needing arms, partly because there are more lower-limb amputations (95 percent of amputees), which means a bigger market for those working to improve the technology. Stockwell’s C-Leg, made by Otto Bock HealthCare in Germany, employs a microprocessor and hydraulics to enable the leg to swing forward automatically once a certain percentage of the wearer´s weight has shifted. The Icelandic company Ossur´s newer Rheo knee is similar to the C-leg, using a microprocessor to sense the knee´s position and load, which allows the leg to adapt to the person´s gait.
But these high-tech replacements can´t tell the wearer where the limb is in space. The devices act in mute isolation, unable to share information with the central nervous system, unable to grasp the user´s desires or even coordinate with the opposite limb. The only way to know whether the C-Leg has negotiated a curb is to look directly at the leg. “Your ankle talks to your other ankle-you´re distributed,” says Herr, one of the Rheo´s inventors. “Amputees are not yet distributed. So if I´m using the Rheo or the C-Leg, and I´m walking along and I see steps up ahead, I have no way to tell my knee that.”
Then there is the pain. Prosthetics can be heavy. If an arm socket is too tight, it pinches; too big, and the prosthetic leg feels unsteady. After six months with her C-Leg, Stockwell still moved in stages-torso, hips, legs-hating it when people stared. She decided to wear shorts, even in winter. “I’d rather they see my legs,” she explains, “than wear pants and have them wondering, ‘What’s wrong with her?'”
Bionics: We Do Not Have the Technology . . . Yet
The higher up the arm or leg someone is amputated, the more flexibility and range of motion disappears. Losing a foot is better than losing a knee; losing a wrist beats missing an elbow. Strip away multiple joints, and the body loses pronation, supination, abduction and adduction–those lovely, complicated multi-joint moves that allow people to sip iced tea or sidestep a pothole, moves that current prosthetics cannot mimic with ease.
As an orthopedist, Roy Aaron understands this. The Brown University Medical School professor was sobered every time he read about soldiers missing arms and legs. Here were lithe, active, determined people in prime physical shape. Years of wearing current prosthetics would leave them crippled with arthritis and other overuse injuries.
Aaron had time to think about this more deeply when his own body crashed. Confined to his bed for a few months in 2004 with a bad back, he dictated notes about a multipronged prosthetics project. The effort would marry tissue engineering, electronics, metallurgy, neurology and robotics, leveraging a toolkit of techniques to create hybrid limbs-part biological, part synthetic-that would one day allow amputees to move supplely and pain-free, their minds and bodies again working together as one. If researchers could replace the lost tissue and nerves and integrate the new flesh with smart, robotic prosthetics that could sense what their wearers´ minds and bodies wanted to do, Aaron thought, these young people could once again move with ease.
Aaron´s timing couldn´t have been better-his vision helped secure some of the new VA funding for the creation of the Center for Restorative and Regenerative Medicine. There, he´s finding ways to save damaged joints and extend the residual limb, commonly called the stump. His quest is for humans to mimic the axolotl, a type of salamander and the highest animal on the evolutionary scale that can regenerate a limb. “Cut a limb off, and he’ll just regenerate a whole arm or whole leg, toes and everything,” he says. “I’ve got to figure out how to talk to these newts and find out how they do it.”
But the marvelous future that this technology promises is too distant to help Halfaker, who worked with a custom-prosthetics designer at Walter Reed to fashion a limb that is light, realistic-looking-and otherwise utterly unfunctional. The designers made a translucent silicone socket liner that hugged her scar and was secured by a bra strap. Onto that they screwed an aluminum rod with tubing that could be bent into several positions. They then added urethane foam padding and, finally, stainless-steel fingers that can be bent into position. Her new arm was hand-painted by a former makeup artist with CSI: Miami to match her other arm, freckles and all. No motors, no sensors, no microprocessor. No utility except psychological: It would fill Halfaker´s sleeve and make her seem, at first glance, complete. “I want to look like I did before,” she says. “Who wouldn’t?”
Melding Body and Bionics
Of the many hurdles on the road to creating a Halfaker-friendly prosthetic, one of the most critical is the socket, the place where flesh and prosthetic meet. There have been plenty of socket innovations, including vacuum sockets that suspend the limb and suction sockets that add or remove fluid to maintain a consistent fit. But the best option would be to get rid of the socket altogether.
In 1952 Swedish orthopedist Per-Ingvar Branemark discovered that a titanium rod inserted in a rabbit´s bone fused well. He called it osseointegration, and the technique has worked wonderfully for dental implants, false teeth built on rods anchored in the patient´s underlying bone. In 1990 Branemark´s son, Rickard, an orthopedic surgeon at Sahlgren University Hospital in Gothenburg, Sweden, surgically implanted rods into human patients´ bones to act as a stable base for a prosthetic arm or leg. But several patients suffered complications. The skin never fused around the rod, acting as if it were a wound, and infections sprouted.
At Brown, molecular biologist Jeffrey Morgan and dean of engineering Clyde Briant are seeking ways to stop such infections. Briant is experimenting with titanium and alloys in search of a combination that is strong yet compatible with human tissue. Morgan is growing skin cells that will cling to the metal, forming a natural seal. It shouldn’t be impossible: “Brown students,” he observes, “have pierced noses.”
Once science figures out better ways to attach artificial limbs, prosthetics themselves need to become smarter, able to act on signals sent directly from the brain. Consider the case of Jesse Sullivan, a power lineman from Dayton, Tennessee, who lost both arms at the shoulder after being electrocuted on the job in 2001. A year later, doctors transferred four nerves (which were no longer infusing muscle) that had controlled his left arm out of his shoulder area and into his pectoral muscles. Six months after that, Todd Kuiken, director of the Rehabilitation Institute of Chicago´s Neural Engineering Center for Artificial Limbs, detected signals in the nerves. Kuiken´s team studded the surface of Sullivan´s chest with electrodes and joined them with wires to a multi-jointed prosthetic. The goal was to connect brain to artificial arm by redirecting signals from Sullivan’s severed nerves. It worked. When doctors asked Sullivan to think about opening his hand, the device, almost instinctively, sprung open. “It was the greatest feeling I’d had since I’d been hurt,” Sullivan says. He can now eat, mow the lawn, and do his laundry, but his arm fulfills only a small fraction of the nerves´ potential power. The nerve for hand closing controls at least 20 muscles, Kuiken says, “and I’m using it for just two different signals. If we tease it out, we might get better and better control.” Kuiken is now developing sensors that will allow Sullivan to feel what he is touching.
Another way to power artificial limbs is to bypass the nerves and tap directly into the brain. That´s what John Donoghue, director of Brown´s Brain Science program and the chief scientific officer at Cyberkinetics Neurotechnology Systems in Foxborough, Massachusetts, is working toward with the invention of BrainGate, a chip that was implanted in 2004 into paralyzed 25-year-old stabbing victim Matt Nagle. With the four-millimeter-square chip in his primary motor cortex, Nagle thinks about moving a cursor on the computer screen to the right. His neurons fire in a certain pattern, and those data are transmitted through a plug affixed to his skull to the computer, which moves the cursor. Soon, BrainGate´s developers got really ambitious. They lay a prosthetic arm, tethered to the computer, on Nagle´s lap and told him to open the hand. He did, just by thinking, and swore in amazement as the hand unfurled. Donoghue promises that future versions will operate wirelessly; Cyberkinetics is developing a control system that uses wireless transmitters and fully implantable power sources.
Fully Wired Limbs
In time, the brain will need to start hearing back from the prosthetics it´s sending signals to. It ordinarily receives a flurry of sensory feedback from a human leg-the terrain being navigated, the pitch of the incline-and can signal adjustments that need to be made. Next-generation prosthetics will be loaded with far more sensors than the Rheo and C-Leg have. They will pick up many, if not all, the cues that biological joints receive and be able to track their own pitch, forward thrust and spatial orientation.
But embedding prosthetics with sensors is useful only if those sensors can communicate with the wearer’s brain and spinal cord. The most promising middleman for such chatter is an invention called artificial nerve cells, or BIONs–”bionic neurons.” Developed by researchers at the Alfred E. Mann Institute at the University of Southern California, these implantable devices (centimeter-long glass capsules equipped with electrodes) have already been successfully injected in or near patients´ muscles and nerves to treat paralysis and to stimulate the limbs of stroke and arthritis patients. The researchers are now working on BION2, which will amplify existing nerve signals-sending instructions to the muscles and pr0cessing feedback from the limb-and might improve communication between a prosthetic limb, such as a hand with moving digits, and its wearer´s brain.
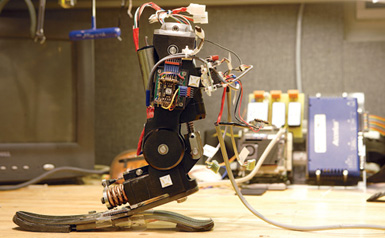
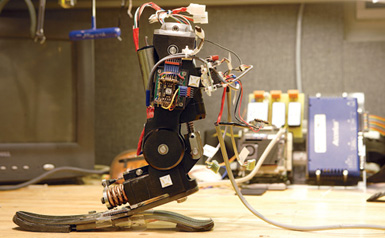
When these sensors determine that a leg needs extra power-for, perhaps, an uphill climb-they might operate in tandem with computer-controlled motors, also integrated into the prosthetic, to give the wearer a boost. Herr and his team have fashioned an “active ankle” that can behave like a spring or add or dissipate energy. His prototype has a motor in the ankle and a series of springs. The wearer would have wireless sensors implanted in his remaining leg muscle that would communicate with the ankle´s internal computer, augmenting power when needed. Herr has tried the device himself and describes it as equivalent to hopping onto a powered airport-terminal walkway. “If it were a product,” he says, “I would call it the Catapult.”
As all these technologies are refined, the artificial limbs will begin to look more and more like human limbs from the outside-and possibly even from the inside, as the human design is geared so well to its many tasks. Multi-jointed fingers will replace hands that have only three unjointed fingers, to achieve more naturalistic dexterity. Mechanical knees and ankles will become progressively more streamlined and efficient. Ultimately, even the means by which the joints are activated will become more humanlike.
Roy Kornbluh, a senior research engineer at SRI International in Menlo Park, California, has been experimenting with an electroactive polymer, also known as artificial muscle, that expands when voltage is applied and contracts when it´s turned off. “The more voltage, the more it stretches,” Kornbluh says. The process mimics human muscle, which changes shape in response to chemical signals.
Thinking Through Every Step
When a soldier loses a leg, she spends hours in physical therapy simply learning to stand. Stockwell started out on crutches. Next she stood using two canes. Then one. She stood on one leg. She stood and threw a ball. Finally, she stood on a C-Leg and hobbled down some parallel bars. In time, she walked free of bars. Then she pulled her seated physical therapist around the room, harnessed like a horse with some long stretchy Therabands. Running is the last step, the ultimate sign of the wearer´s success at managing body-machine mechanics. She had tried to run on a leg without an artificial knee, which forced her to kick with a circular eggbeater motion. The effort exhausted her.
Her prosthetist, Elliot Weintrob, had another idea. One brisk day in early spring last year, Weintrob, Stockwell and her husband, Dick, who is also a soldier, drove to a track in northern Virginia. Stockwell slipped into a socket consisting of an Ossur Total Knee attached to a bouncy Ossur Flex-Run Foot, a spring shaped like a large upside-down question mark. The knee could swing forward freely but did not have the C-leg´s ability to catch and lock if she started to fall.
“I’m scared,” Stockwell said to her husband. She tucked some hair behind her ear.
“You can do it,” he replied softly. They walked to a middle lane and he whispered in her ear, “Take off!”
She took six choppy long steps, her prosthetic leg flapping forward. Out of habit, she made the eggbeater motion. Weintrob pointed this out.
“I feel better,” she said hopefully. She started again, an awkward rise and collapse to her gait. She stopped, her face flushed, tendrils of hair twirling around her face. She started again. You could tell it hurt by the quick, short steps she took, her arms pinched against her body. She ran like she had stubbed her toe-over and over again.
Eventually, she got the hang of it. Months later, she managed to make her leg work well enough to compete in road races and triathlons, where she uses an arm-cranked bike. Last fall, inspired by her experiences, Stockwell began studying prosthetics at a Minnesota college, all the while convinced that her chosen field will ultimately become obsolete. A century from now, she says excitedly, prosthetics won´t be necessary: Doctors will be regenerating limbs!
At the track last spring, though, her back was sore, her backside was chafed, and she was tired of thinking about where to place her left leg next. “Every step,” she said. “I think about every step.”
Suzanne Sataline is a Wall Street Journal reporter in Boston.




