
A challenging operation for any surgeon to perform is to repair a hole in an organ—such as a tiny defect in the heart or a tear in the stomach wall caused by an ulcer. These problems are often life-threatening and require surgery. Even when a noninvasive technique is used, the patient is often left with a metal-based device permanently plugged into the hole, which, overtime, can erode the natural tissue surrounding the area. But researchers at Harvard University have come up with an alternative: A way to repair these holes using a minimally invasive catheter device, a pair of balloons, and UV light-activated glue. Their work was published today in Science Translational Medicine.
The new method is the first to combine the catheter and balloon technique with the light-activated glue, which was developed last year by the same researchers. The glue works via an adhesive-coated patch made of biodegradable materials, which attaches to the perforated area—whether it is in the heart, stomach, intestines, or another organ—and serves as a scaffold to allow the tissue to grow and heal. Once the tissue has completely healed, the patch melts away. Since this UV light-activated adhesion method was developed, the researchers had trouble finding a way to get the adhesive patch to the affected area without using invasive techniques like surgery.
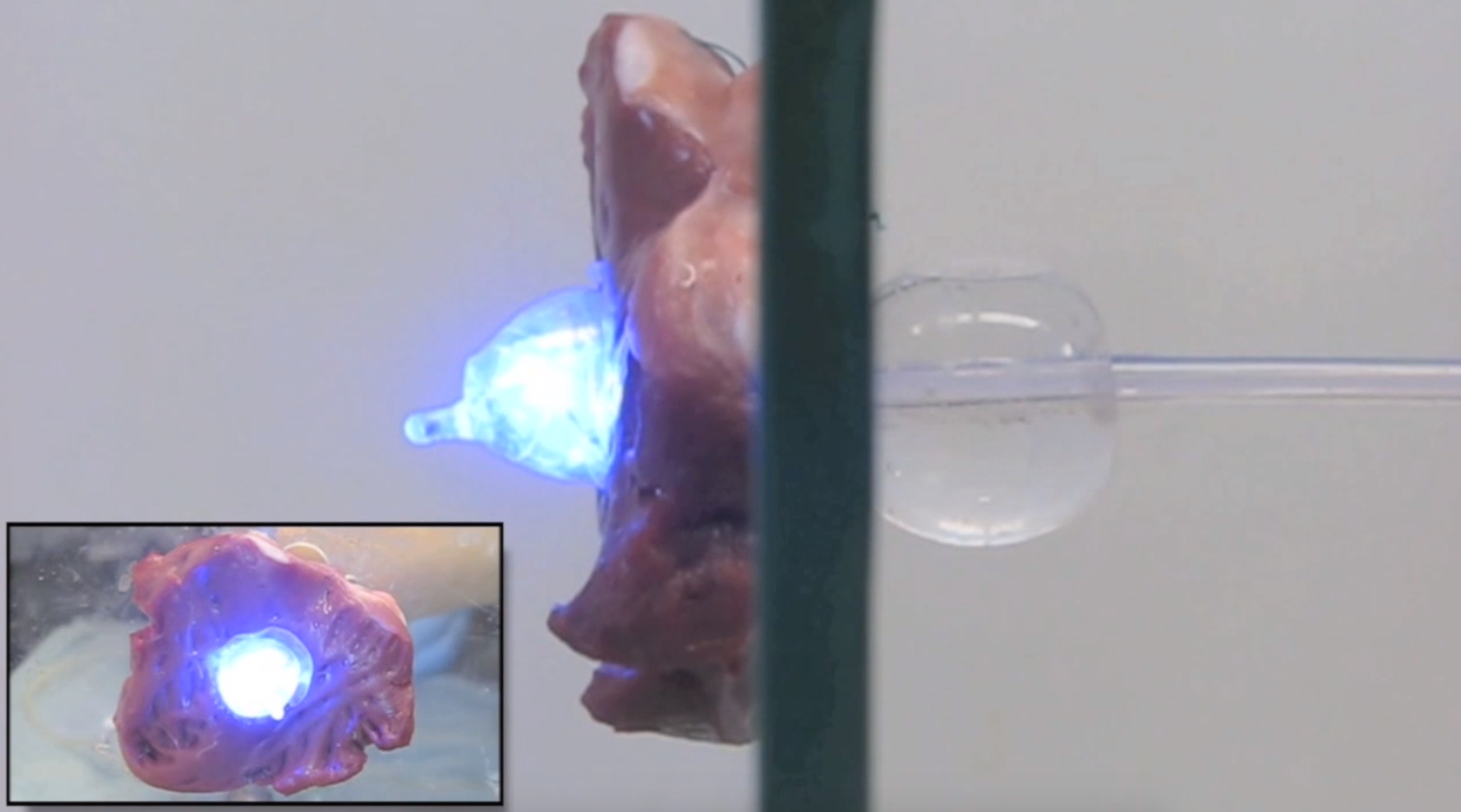
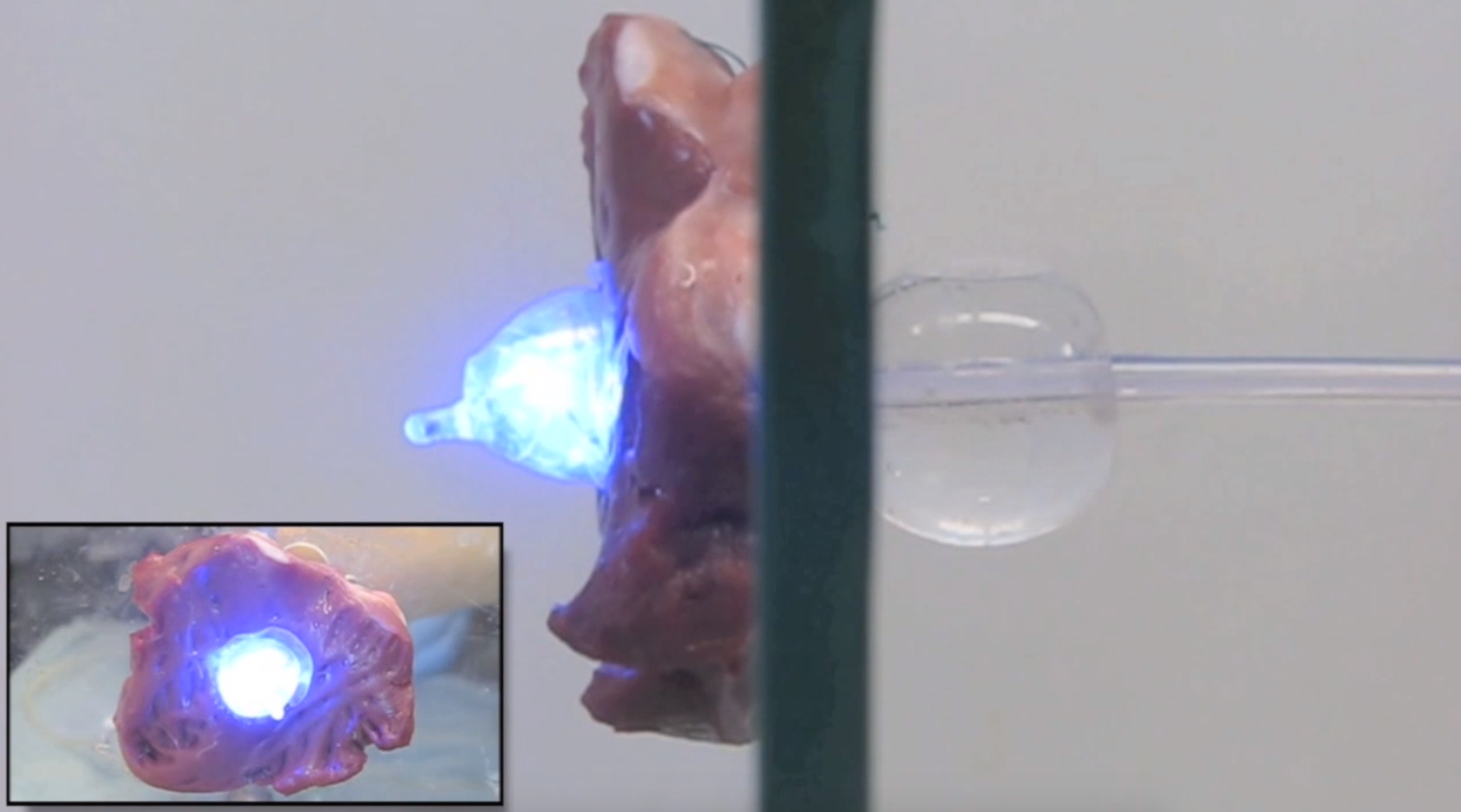
Their new technique uses a thin hollow plastic tube called a catheter to guide the patch to its destination. During the procedure, the catheter is first advanced to the organ (either through an endoscope to digestive organs or through a catheter to the heart or bladder) and then slowly guided through the perforation or defect. Once that’s secure, a system of two balloons helps put the patch in place. First the balloon on the outside of the organ inflates, which deploys the adhesive patch onto the affected area. Then a balloon on the inside of the organ is inflated, which causes the ultraviolet light to turn on. This activates the adhesive properties of the glue and forces the patch to stick onto the tissue. Once finished, the balloons deflate and the catheter is removed. The patch sits on the hole until the tissue heals itself. Once it’s done, the patch dissolves.
See the procedure done on a defect in a pig heart tissue sample, in GIF form:
Credit: Roche et al., Science Translational Medicine (2015), C. Schaffer/AAAS
The entire process is fast—the maximum wait time for the adhesive material to activate and do its job is about two minutes. The researchers hope this new catheter-guided technique will allow the light-activated adhesives to be used more readily and with less invasive procedures. Particularly, they envision this device to be especially useful for closing tiny holes in the heart, which right now requires the patient to undergo a highly invasive cardiopulmonary bypass procedure.

When put to the test, the new technique worked just as well as a traditional invasive suture technique in healing perforations in the stomach, abdominal wall, and heart tissue of rodents and pigs. Further, they tested its ability to close a septal wall defect in the beating heart of a pig—which showed that it could withstand high-pressure blood flow.
Devices for body defect closures using a catheter as a guide have been proposed before, however, the researchers note, they have almost exclusively relied on metal-based material and require a mechanical or a suture attachment, which overtime can erode tissue.
The use of this new method in real patients is still far off, however, as the point of this early study was simply a proof of concept. The initial experiments did show some limitations, including the flexibility of the catheter device. In future studies, the researchers hope to use multiple fiber bundles and a cone-shaped tip to increase flexibility and access, which they hope will bring the device closer to being ready for clinical use.
