From cities in the sky to robot butlers, futuristic visions fill the history of PopSci. In the Are we there yet? column we check in on progress towards our most ambitious promises. Read more from the series here.
From tar, animal fat, and gold wires to painted polymethyl methacrylate, or Plexiglas, the nearly 5,000-year journey to perfect prosthetic eyes has been an odyssey through the periodic table. It has also been an art story.
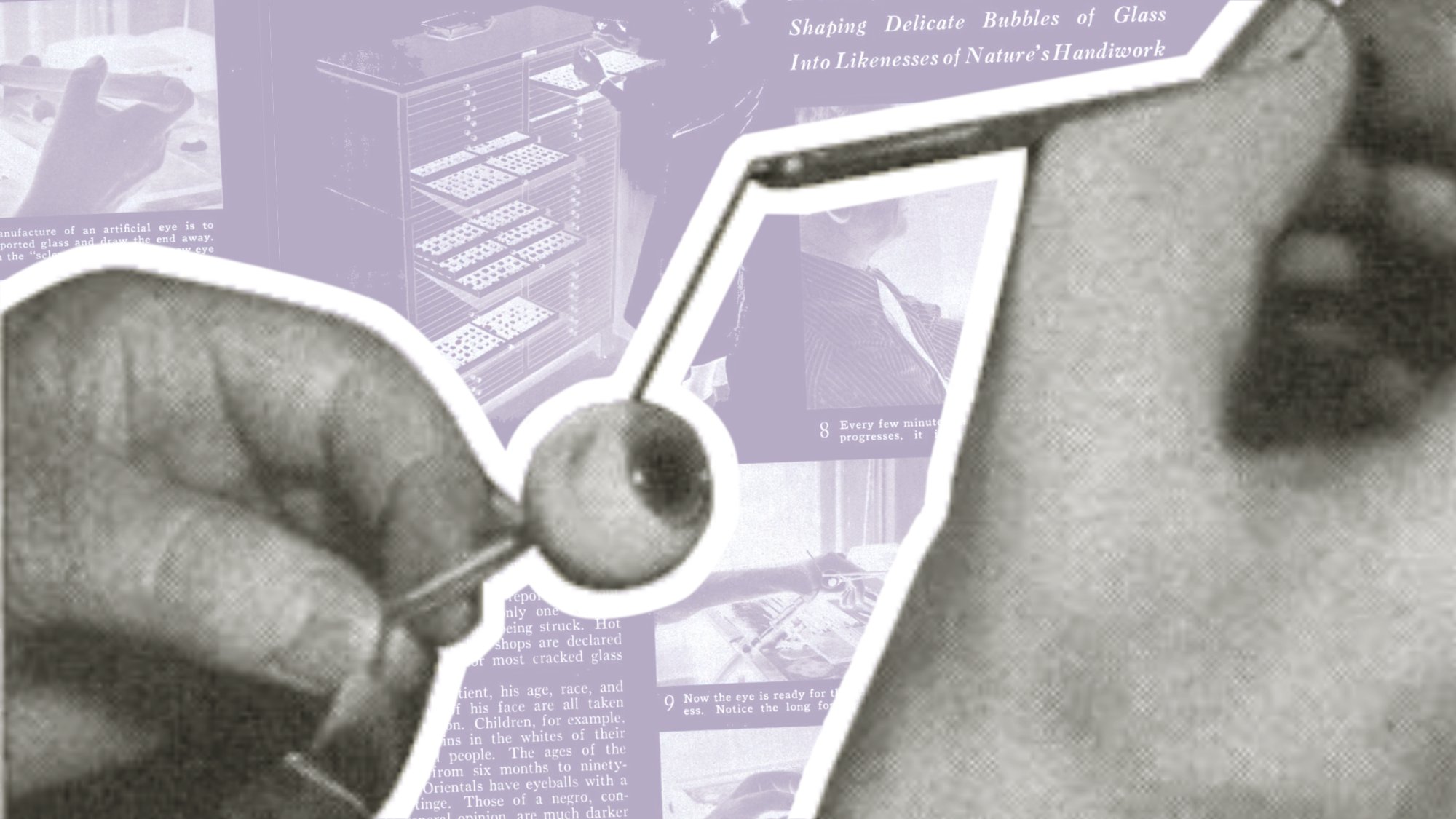
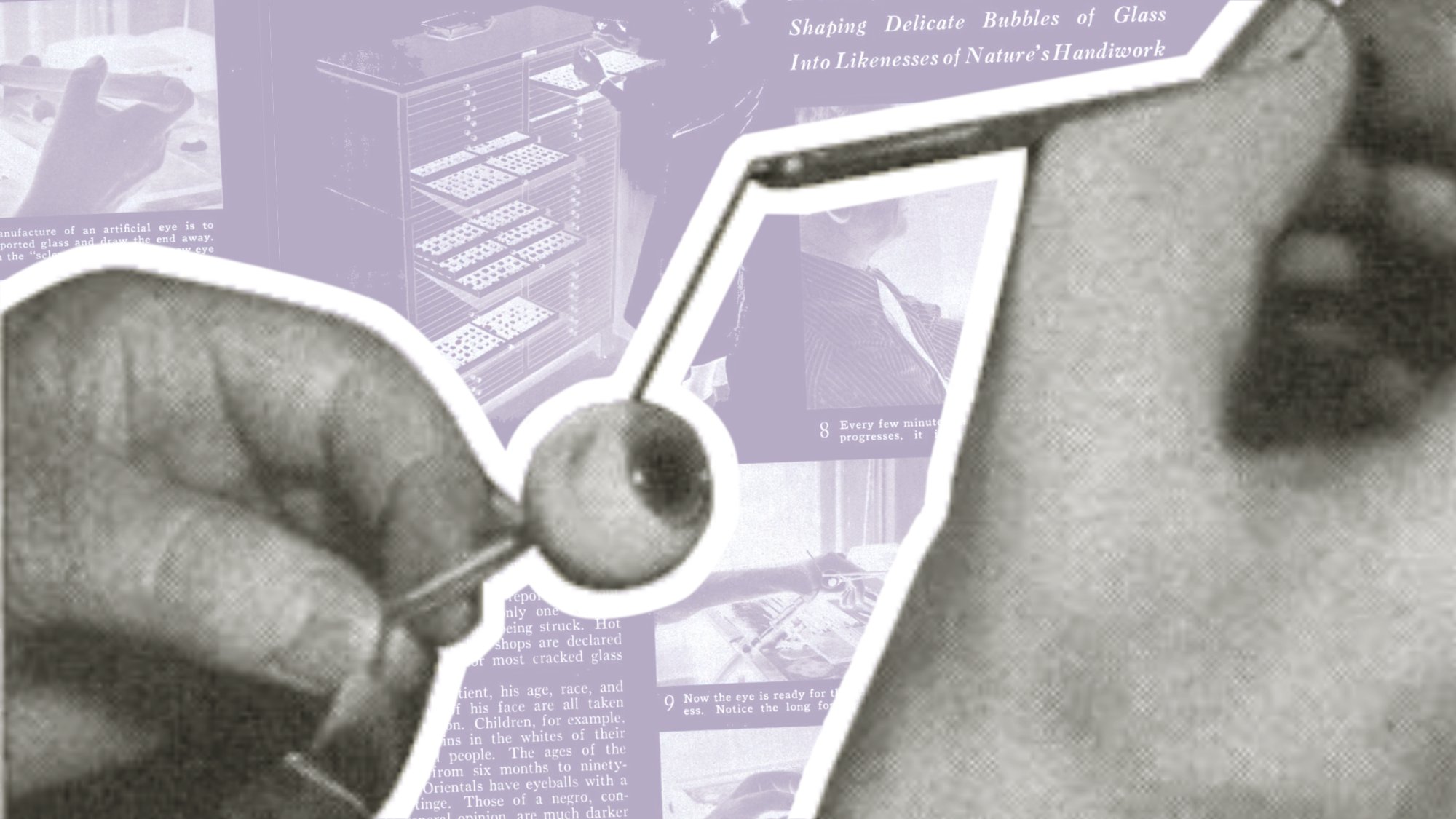
In July 1937, Popular Science described the art of making artificial eyes using glass-blowing techniques that can be traced back to 16th-century Venetian glassblowers. The glass used in 1937 was a special stock imported from Germany. Its unusual properties derived from the work of early 19th century dollmakers, who had learned to produce realistic eyes by infusing glass with cryolite, a milky-white mineral of sodium, aluminum, and fluoride first found in Greenland. When World War II got underway, however, German cryolite glass exports came to a grinding halt, forcing prosthetic eye makers to hunt for new glass sources and new materials.
Enter polymethyl methacrylate, or PMMA, an acrylic first used in dentistry. Even though PMMA has remained the most widely used prosthetic eye material since the 1940s, artificial eye technology has not stood still. New materials, parts, tools, and processes have improved upon appearance, comfort, function, and cost, including, most recently, 3D printing.
On becoming an ocularist
Whether they used tar, clay, wood, metal, stone, glass, or acrylic, what has bound prosthetic eye makers, or ocularists, across the millennia is their artistry. Medium notwithstanding, making artificial eyes requires lots of practice and the ability to mold, sculpt, and paint.
“It is very much a generational career,” according to Lindsay Pronk, an ocularist at the University of Iowa Hospitals and Clinics. “You have family lines. My step dad taught me,” she says. “I have a friend in New Jersey, she’s third generation and still working with her dad whose cousin is on the west coast training his son, who will be fifth generation.” Pronk explains that to become an ocularist doesn’t require a university degree, but rather “a five year apprenticeship—three years on the job training, and two years making eyes,” for a total of about 10,000 hours. Many universities offer accredited ophthalmic technician training programs for students who want to assist ophthalmologists, but there is no specific program for ocularists. The American Society of Ocularists does, however, administer its own College of Ocularistry, and, along with other professional organizations, offers board certification, which requires passing a written and practical exam. Pronk is a board-certified ocularist (BCO). As of 2022, there were about 170 BCOs practicing in the United States.
Tracing the evolution
The oldest known artificial eye—a 4,800-year-old orb with a dark central circle spoked by golden threads—was discovered in 2006 at an archaeological site in Iran. Ancient Romans and Egyptians made eyepatch-style prosthetics of painted clay and leather straps. In 16th-century Europe, wood and ivory may have been the first materials used for in-socket artificial eyes, followed by enamel-coated gold and silver. But it was Venetian glass-blowers who elevated prosthetic eyes to a realistic level, sparking centuries of glass-eye innovation that improved upon appearance and comfort.

Given how important eye contact is as a form of human communication, the quest for realistic prosthetic eyes is not surprising. In a study published in PLoS One in 2016, researchers from France and Switzerland determined that direct eye contact with someone triggers a series of brain activities that tune us into the other’s presence. And in a study published in 2024, researchers corroborated what other recent studies have reported—that eye contact is one of the chief cues associated with romantic attraction and a sense of closeness. When it comes to prosthetics, artificial eyes may directly affect the quality of social relationships even though they can’t restore sight. Which is why, beyond appearance, motility is so important. Even the most realistic artificial eye will stand out if it is motionless or out-of-synch with the working eye.

Improving motion through implants
Today, we take anesthesia for granted, but until the late 19th century, surgeries were performed without anesthesia. For ocular surgeries, which were particularly gruesome and painful, that meant enucleation (removal of the entire eyeball) or evisceration (removal of eye contents, leaving the sclera intact) were performed as a last resort. Glass eyes were typically hollow scleral shells that slipped under the eyelids and rested on the existing, nonfunctional eye. But its movement was limited because it was not attached.
It was in 1885 that Philip Henry Mules, an English ophthalmologist, performed the first known evisceration followed by an orbital implant, a marble-size glass sphere inserted in the eye socket, or clerical cavity, to restore the overall shape and volume of the eye. The glass prosthetic shell then rested on the implant instead of the eye. Although Mules’s implant was not attached to the orbital muscles (nonintegrated), it still rotated slightly with the socket’s soft tissue. The orbital implant procedure set off a new chapter in artificial eyes.
A story published in LIFE in December 1948 offered vivid depictions of a procedure, pioneered by researchers in Boston, to fit a ball-shaped, pegged ocular implant in the eye socket. By attaching the pegged implant to orbital muscles, the ball could rotate in tandem with the working eye. A removable prosthetic eye snapped into place on the pegged implant and could be replaced as needed. But the implant’s acrylic and metal mesh materials—also known as inert materials—used in the procedure proved to be unstable because the muscles would detach; and with the peg, the socket was prone to infection.
Such integrated implants were largely abandoned until the 1980s when a new biointegrated material, hydroxyapatite—derived from ocean coral—replaced acrylic, reviving the procedure. It was ocean coral’s porous features that stimulated soft-tissue growth, enhancing the implant’s integration, making it more stable. But ocean coral was a bit rough, so other similarly porous materials followed, like porous polyethylene and aluminum oxide.
According to Pronk, most implants are now fully integrated using porous acrylic. “They still attach the four muscles to the ball of that implant,” she explains, “and then sew the tissue over it. All that tissue then grows into the implant, making it fully integrated.” About six weeks following orbital implant surgery, Pronk steps in. With the same material used by dentists, she makes a mold of the eye to create a bespoke prosthetic. In the US, Pronk claims that all artificial eyes are made of PMMA and have been for some time. “I don’t believe there’s anyone in the US that does glassblowing.”
Besides hand painting the iris to match the working eye, which takes about six hours, Pronk spends time adjusting the curvature of the prosthetic to ensure that it is similar. Comfort is key, as well as “making sure we get as much movement out of it as we can.”
Declining demand is a good thing
According to the United States Eye Injury Registry, which has not been maintained for more than a decade, there were an estimated 2.5 million eye injuries in the US each year and 50,000 people permanently lost part or all of their vision. Such data is not directly collected today, but organizations like the American Academy of Ophthalmology still cite those statistics as a gauge of demand for certain eye healthcare services, among them, the ocularists who make custom prosthetic eyes.
During her 18 years as an ocularist, however, Pronk believes that the demand for prosthetic eyes has declined, which is consistent with systematic reviews of global blindness trends. She cites improvements in workplace safety laws as well as advances in surgical procedures to save eyes that have endured injury or trauma.
Even though the process of making prosthetic eyes—taking molds, casting the acrylic, hand painting the iris, and polishing—has remained largely the same for decades, technological innovation has not stood still. Some ocularists are turning to digital photography to capture images of the iris, which is printed on a special adhesive paper and embedded in the prosthetic. And in 2021, a UK patient at University College London was the first to be fitted with a custom 3D-printed eye. In a study published in Nature Communications in 2024, researchers from Germany and the UK evaluated an automated process of scanning, fitting, and printing 3D prosthetic eyes on 10 patients. While patients gave high ratings to the quality of the printed eyes, the process still required the skills of an ocularist to make final adjustments and sometimes even shape the artificial eye. Turns out, even with automation there is still an art to making realistic artificial eyes.
While Pronk thinks there’s a role for digital imaging in making prosthetic eyes, she’s not convinced that the technology involved in 3D printing, which starts with scanning the eye socket, offers much improvement over the traditional process. Plus, the equipment is expensive. She’s also not convinced that printing—either 2D or 3D—can yet match the intricacy of hand-painted irises.
When it comes to art, Pronk confesses that she cannot draw to save her life. But she loves painting irises, which involves paying attention to the smallest details, and building it up layer by layer to “give a better illusion of depth.”
As for future technological advancements, Pronk doesn’t anticipate significant changes in how prosthetic eyes are made, but she is encouraged by some of the progress in artificial eyesight by companies like Elon Musk’s Neuralink. But she wonders if eye transplants might come first. “Much like how they do a liver transplant,” she says. “At that point, you know, I’ll be out of a job. But it’s a pretty great reason to be out of a job.”
