This article was originally featured on ProPublica. ProPublica is a Pulitzer Prize-winning investigative newsroom. Sign up for The Big Story newsletter to receive stories like this one in your inbox.
The outbreaks keep coming.
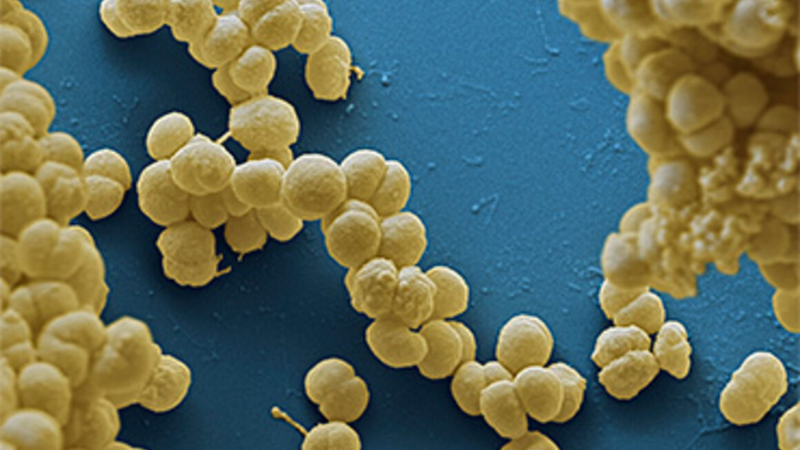
Mpox, the virus formerly known as monkeypox, last year crossed borders with unprecedented speed to infect nearly 90,000 people. In the past year, Ebola killed at least 55 in Uganda, and a related, equally deadly virus called Marburg emerged in two countries that have never seen it before. Now, scientists are worried that a dangerous bird flu that’s been jumping to mammals could mutate and spread among humans.
These viruses all came from wildlife. Understanding what conditions prime pathogens to leap from animals to people could help us prevent outbreaks. After COVID-19 showed the world the devastation a pandemic can bring, you’d think this type of research would be among the hottest areas of science, with funders lined up far and wide.
That’s not the case. As ProPublica has shown in a series of stories this year, global health authorities focus far more attention and money on containing outbreaks once they begin rather than preventing them from starting in the first place. This mindset has hindered scientists who study the complex dynamics that drive what’s known as spillover, the moment a pathogen leaps from one species to another.
Australian researcher Peggy Eby and her colleagues have shown that it is possible to predict when spillovers are going to happen by closely tracking bats that spread contagion and patiently observing changes that shape their world. This groundbreaking research on the often-fatal Hendra virus relied on decades of Eby’s field work, some of which she did without pay. Early on, one government funder told her that the project she proposed wasn’t a “sufficiently important contribution.” She and her colleagues had to cobble together a mishmash of different grants and keep impatient funders happy. Their work, published late last year in the journal Nature, highlights ways to intervene and potentially prevent outbreaks.
Scientists want to unlock similar mysteries involving other infectious diseases, but research like this is difficult to do and even more difficult to fund. Here are some of the obstacles that stand in the way:
High-tech research overshadows old-school field work.
Government and scientific funding organizations typically reward cutting-edge technologies, such as using machine learning to build models. But those are only as good as the information fed into them — data that someone like Eby has to collect through painstaking groundwork. Many of Eby’s most important insights have come from visiting and revisiting bat roosts over many years, and there was nothing high-tech or novel about her method: a keen eye, a pair of binoculars, a pen and a notebook.
Funders prize novelty over exploring existing theories.
Some funders prioritize totally new ideas. Eby and her colleagues have found that bats shed more Hendra virus after being stressed by food shortages, which have increased as people cut down native trees that once provided the nectar the bats like to eat. Sarah Olson, director of health research at the Wildlife Conservation Society, has long wanted to conduct similar research on bats suspected of carrying the Ebola virus in the Republic of Congo. Developers have cleared swaths of forest in recent years to build roads and housing, and Olson wants to understand how that’s affected these bats.
Olson has applied for grant after grant since 2015 but has struggled to get sufficient funding. Even before she applied, an employee at the National Science Foundation told her the study wouldn’t be novel enough because she wasn’t exploring an entirely new theory. Rather than strengthening her case, Eby and her colleagues’ prior work weakened Olsen’s chances. A spokesperson for the National Science Foundation said the agency could not comment on specific grants. Speaking generally, the spokesperson wrote, “The most competitive proposals are those that advance broad, conceptual knowledge that reaches beyond the specific system under study.”
Olson has lined up Congolese researchers who are willing to collaborate. “We can do it,” she said. “It’s just a matter of getting funding and the interest.”
Funders’ focus is often too narrow.
If you want to predict and prevent an outbreak, you have to answer big questions: What causes spillover? Why this year and not another? How does a changing environment influence animals and their interactions with humans? Experts across disciplines are needed, but cross-disciplinary vision is hard to find among many of the most prominent funding agencies.
The National Institute of Allergy and Infectious Diseases, for example, focuses on research to develop treatments, vaccines and diagnostic tests and to understand viruses at the molecular level. Conservation and environment-focused grants rarely include human health in their scope.
Olson pitched her study on Congolese bats to the National Institutes of Health. She got rejected, she said, because grant reviewers said that it wasn’t clear how the bat results could be linked to human infections. An NIH spokesperson said the agency doesn’t comment on specific grants, adding, “It is incumbent on investigators who want to study overlapping interests of animal and human health to clearly describe the relevance of their proposed research to the advancement of human health.”
Eby and her colleague, Dr. Raina Plowright, a professor of disease ecology at Cornell University, smacked into these same silos when their applications for grant after grant were shot down. An animal foundation, for instance, said it wasn’t within its mandate to care about diseases that jumped to humans.
Thomas Gillespie, a professor of environmental sciences at Emory University, wanted to investigate whether stress affects when cave-dwelling bats in Costa Rica shed leptospirosis, a type of bacteria that can be deadly to humans. A joint program from the National Science Foundation and the NIH said the project was “too ambitious,” he recalled. Gillespie and his colleagues tried for a different NIH grant, but reviewers complained the focus was too much on animals and not enough on humans, he said. In the end, he and his colleagues stitched together funding from a museum, a nonprofit and private foundations, but they had to scale back the project to stay within budget.
Long-term research doesn’t fit into short-term grants.
Research grants typically last two to three years, which is not enough time to observe how climate change, food shortages, habitat loss and deforestation are affecting animal behavior. For their Hendra research, Eby and her colleagues analyzed data that spanned 25 years. To support that long-term data collection, Eby sometimes took on contract work, such as helping local governments figure out how to deal with bats that people in the area considered a nuisance.
Plowright won a grant from an arm of the Department of Defense, but it only allowed two years for collecting field data. “They needed us to wrap things up and show results to justify our funding,” Plowright said. That schedule is the norm, not an outlier, in science.
Some key programs are one-offs.
It’s not just that grants are short term. Some of the rare grant-giving initiatives that focus on prevention don’t last long either.
The Hendra virus researchers received some of their biggest financial support from a Defense Advanced Research Projects Agency program that was unique in its scope and vision. Called Preventing Emerging Pathogenic Threats, the program sought to understand the reasons contagions spread from animals to people. The ultimate goal was to devise strategies to protect U.S. troops in places where there are endemic and emerging infectious diseases, according to Kristen Jordan, the deputy director for the DARPA Biological Technologies Office. Unlike many others, this program was designed to support multidisciplinary research and was squarely focused on prevention. In 2018, it funded five projects, including the Hendra virus research.
But that’s it. After five years, the program is wrapping up for good. “We look to our government partners to pick up the pieces, if they so desire,” Jordan said. “We are ready for the next hard problem; there are many we need to address.”
Similarly, a program at the NIH called the Centers for Research in Emerging Infectious Diseases is among the few that fund scientists across disciplines who are trying to understand spillover. Established in 2020, the program plans to award $82 million over five years. That’s not as much as it sounds. Consider that the NIH receives more than $3 billion annually for HIV and AIDS research. Jean Patterson, the scientist who helps oversee the program, said that when the five years is up, she and her team have to make the case to NIH leaders that their program should continue or it will be dropped.
Money is scarce, even for solutions.
When researchers uncover ways to prevent outbreaks, getting funders to implement those solutions is no sure bet. Emily Gurley, an infectious disease epidemiologist at Johns Hopkins University, succeeded in winning government funding to piece together how the Nipah virus jumped from bats to people in Bangladesh. She and her colleagues figured out a way to interrupt the transmission of Nipah, the virus used as the model for the disease in the movie “Contagion.”
Gurley and her team used infrared cameras to determine that bats were drinking sap that residents were collecting in pots attached to date palm trees. People caught Nipah when they drank sap contaminated by infected bats.
Across multiple studies, Gurley and her colleagues showed that bamboo skirts covering the pots were cheap and easy to make, accepted by local sap collectors and effective at keeping out bats. With a proven solution in hand, Gurley wanted to roll this out in other parts of Bangladesh where bats spread Nipah, but she said no U.S. or international agency would step up to fund that work. The Bangladeshi government tells people not to drink raw sap, but this is a long-standing tradition that may be hard to eliminate.
Gillespie, the Emory professor, said that government and private scientific funding groups need to prioritize research into prevention, so we can learn how best to head off deforestation, habitat loss and other causes of spillover. “We have to do something now, or we’ll end up in an era of pandemics,” he warned.